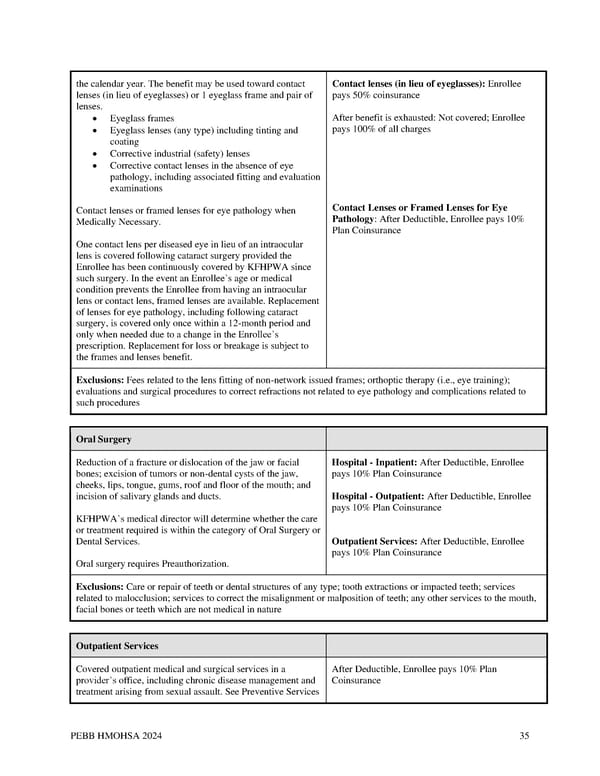
the calendar year. The benefit may be used toward contact Contact lenses (in lieu of eyeglasses): Enrollee lenses (in lieu of eyeglasses) or 1 eyeglass frame and pair of pays 50% coinsurance lenses. • Eyeglass frames After benefit is exhausted: Not covered; Enrollee • Eyeglass lenses (any type) including tinting and pays 100% of all charges coating • Corrective industrial (safety) lenses • Corrective contact lenses in the absence of eye pathology, including associated fitting and evaluation examinations Contact lenses or framed lenses for eye pathology when Contact Lenses or Framed Lenses for Eye Medically Necessary. Pathology: After Deductible, Enrollee pays 10% Plan Coinsurance One contact lens per diseased eye in lieu of an intraocular lens is covered following cataract surgery provided the Enrollee has been continuously covered by KFHPWA since such surgery. In the event an Enrollee’s age or medical condition prevents the Enrollee from having an intraocular lens or contact lens, framed lenses are available. Replacement of lenses for eye pathology, including following cataract surgery, is covered only once within a 12-month period and only when needed due to a change in the Enrollee’s prescription. Replacement for loss or breakage is subject to the frames and lenses benefit. Exclusions: Fees related to the lens fitting of non-network issued frames; orthoptic therapy (i.e., eye training); evaluations and surgical procedures to correct refractions not related to eye pathology and complications related to such procedures Oral Surgery Reduction of a fracture or dislocation of the jaw or facial Hospital - Inpatient: After Deductible, Enrollee bones; excision of tumors or non-dental cysts of the jaw, pays 10% Plan Coinsurance cheeks, lips, tongue, gums, roof and floor of the mouth; and incision of salivary glands and ducts. Hospital - Outpatient: After Deductible, Enrollee pays 10% Plan Coinsurance KFHPWA’s medical director will determine whether the care or treatment required is within the category of Oral Surgery or Dental Services. Outpatient Services: After Deductible, Enrollee pays 10% Plan Coinsurance Oral surgery requires Preauthorization. Exclusions: Care or repair of teeth or dental structures of any type; tooth extractions or impacted teeth; services related to malocclusion; services to correct the misalignment or malposition of teeth; any other services to the mouth, facial bones or teeth which are not medical in nature Outpatient Services Covered outpatient medical and surgical services in a After Deductible, Enrollee pays 10% Plan provider’s office, including chronic disease management and Coinsurance treatment arising from sexual assault. See Preventive Services PEBB HMOHSA 2024 35
 Kaiser Permanente WA CDHP EOC (2024) Page 34 Page 36
Kaiser Permanente WA CDHP EOC (2024) Page 34 Page 36