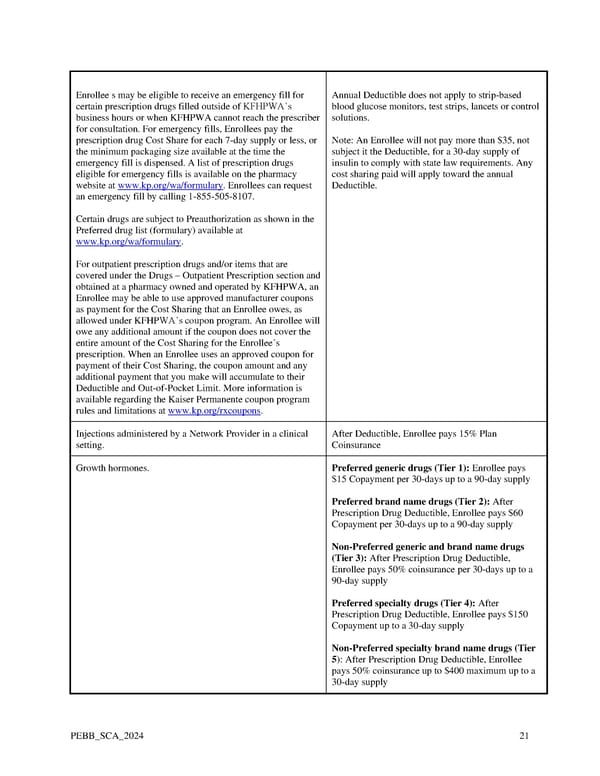
Enrollee s may be eligible to receive an emergency fill for Annual Deductible does not apply to strip-based certain prescription drugs filled outside of KFHPWA’s blood glucose monitors, test strips, lancets or control business hours or when KFHPWA cannot reach the prescriber solutions. for consultation. For emergency fills, Enrollees pay the prescription drug Cost Share for each 7-day supply or less, or Note: An Enrollee will not pay more than $35, not the minimum packaging size available at the time the subject it the Deductible, for a 30-day supply of emergency fill is dispensed. A list of prescription drugs insulin to comply with state law requirements. Any eligible for emergency fills is available on the pharmacy cost sharing paid will apply toward the annual website at www.kp.org/wa/formulary. Enrollees can request Deductible. an emergency fill by calling 1-855-505-8107. Certain drugs are subject to Preauthorization as shown in the Preferred drug list (formulary) available at www.kp.org/wa/formulary. For outpatient prescription drugs and/or items that are covered under the Drugs – Outpatient Prescription section and obtained at a pharmacy owned and operated by KFHPWA, an Enrollee may be able to use approved manufacturer coupons as payment for the Cost Sharing that an Enrollee owes, as allowed under KFHPWA’s coupon program. An Enrollee will owe any additional amount if the coupon does not cover the entire amount of the Cost Sharing for the Enrollee’s prescription. When an Enrollee uses an approved coupon for payment of their Cost Sharing, the coupon amount and any additional payment that you make will accumulate to their Deductible and Out-of-Pocket Limit. More information is available regarding the Kaiser Permanente coupon program rules and limitations at www.kp.org/rxcoupons. Injections administered by a Network Provider in a clinical After Deductible, Enrollee pays 15% Plan setting. Coinsurance Growth hormones. Preferred generic drugs (Tier 1): Enrollee pays $15 Copayment per 30-days up to a 90-day supply Preferred brand name drugs (Tier 2): After Prescription Drug Deductible, Enrollee pays $60 Copayment per 30-days up to a 90-day supply Non-Preferred generic and brand name drugs (Tier 3): After Prescription Drug Deductible, Enrollee pays 50% coinsurance per 30-days up to a 90-day supply Preferred specialty drugs (Tier 4): After Prescription Drug Deductible, Enrollee pays $150 Copayment up to a 30-day supply Non-Preferred specialty brand name drugs (Tier 5): After Prescription Drug Deductible, Enrollee pays 50% coinsurance up to $400 maximum up to a 30-day supply PEBB_SCA_2024 21
 Kaiser Permanente WA SoundChoice EOC (2024) Page 20 Page 22
Kaiser Permanente WA SoundChoice EOC (2024) Page 20 Page 22