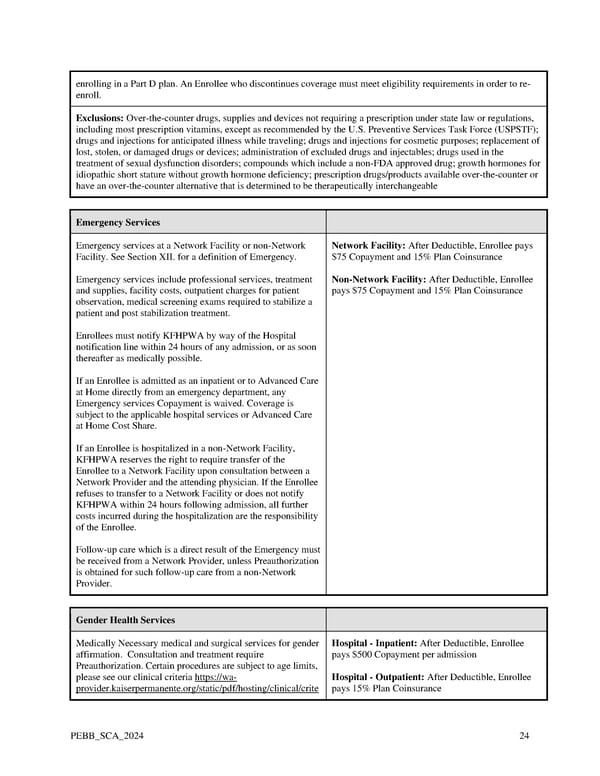
enrolling in a Part D plan. An Enrollee who discontinues coverage must meet eligibility requirements in order to re- enroll. Exclusions: Over-the-counter drugs, supplies and devices not requiring a prescription under state law or regulations, including most prescription vitamins, except as recommended by the U.S. Preventive Services Task Force (USPSTF); drugs and injections for anticipated illness while traveling; drugs and injections for cosmetic purposes; replacement of lost, stolen, or damaged drugs or devices; administration of excluded drugs and injectables; drugs used in the treatment of sexual dysfunction disorders; compounds which include a non-FDA approved drug; growth hormones for idiopathic short stature without growth hormone deficiency; prescription drugs/products available over-the-counter or have an over-the-counter alternative that is determined to be therapeutically interchangeable Emergency Services Emergency services at a Network Facility or non-Network Network Facility: After Deductible, Enrollee pays Facility. See Section XII. for a definition of Emergency. $75 Copayment and 15% Plan Coinsurance Emergency services include professional services, treatment Non-Network Facility: After Deductible, Enrollee and supplies, facility costs, outpatient charges for patient pays $75 Copayment and 15% Plan Coinsurance observation, medical screening exams required to stabilize a patient and post stabilization treatment. Enrollees must notify KFHPWA by way of the Hospital notification line within 24 hours of any admission, or as soon thereafter as medically possible. If an Enrollee is admitted as an inpatient or to Advanced Care at Home directly from an emergency department, any Emergency services Copayment is waived. Coverage is subject to the applicable hospital services or Advanced Care at Home Cost Share. If an Enrollee is hospitalized in a non-Network Facility, KFHPWA reserves the right to require transfer of the Enrollee to a Network Facility upon consultation between a Network Provider and the attending physician. If the Enrollee refuses to transfer to a Network Facility or does not notify KFHPWA within 24 hours following admission, all further costs incurred during the hospitalization are the responsibility of the Enrollee. Follow-up care which is a direct result of the Emergency must be received from a Network Provider, unless Preauthorization is obtained for such follow-up care from a non-Network Provider. Gender Health Services Medically Necessary medical and surgical services for gender Hospital - Inpatient: After Deductible, Enrollee affirmation. Consultation and treatment require pays $500 Copayment per admission Preauthorization. Certain procedures are subject to age limits, please see our clinical criteria https://wa- Hospital - Outpatient: After Deductible, Enrollee provider.kaiserpermanente.org/static/pdf/hosting/clinical/crite pays 15% Plan Coinsurance PEBB_SCA_2024 24
 Kaiser Permanente WA SoundChoice EOC (2024) Page 23 Page 25
Kaiser Permanente WA SoundChoice EOC (2024) Page 23 Page 25