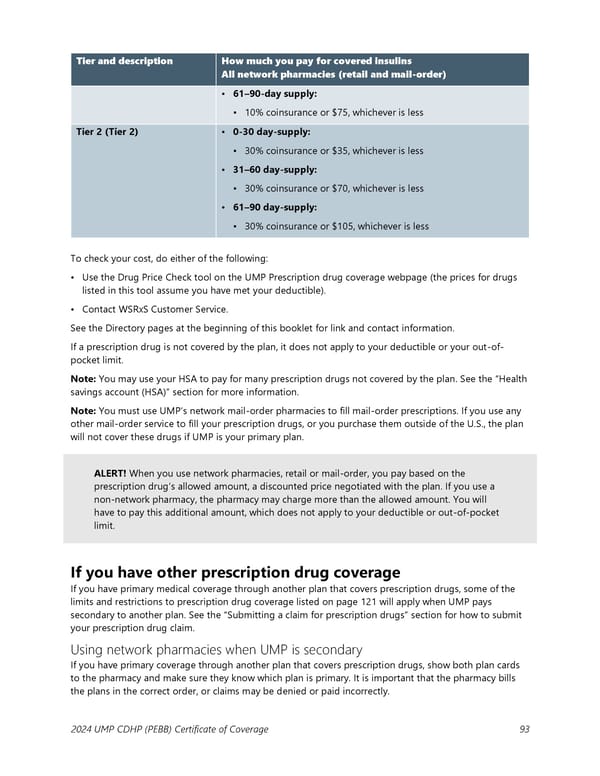
Tier and description How much you pay for covered insulins All network pharmacies (retail and mail-order) • 61–90-day supply: ▪ 10% coinsurance or $75, whichever is less Tier 2 (Tier 2) • 0-30 day-supply: ▪ 30% coinsurance or $35, whichever is less • 31–60 day-supply: ▪ 30% coinsurance or $70, whichever is less • 61–90 day-supply: ▪ 30% coinsurance or $105, whichever is less To check your cost, do either of the following: • Use the Drug Price Check tool on the UMP Prescription drug coverage webpage (the prices for drugs listed in this tool assume you have met your deductible). • Contact WSRxS Customer Service. See the Directory pages at the beginning of this booklet for link and contact information. If a prescription drug is not covered by the plan, it does not apply to your deductible or your out-of- pocket limit. Note: You may use your HSA to pay for many prescription drugs not covered by the plan. See the “Health savings account (HSA)” section for more information. Note: You must use UMP’s network mail-order pharmacies to fill mail-order prescriptions. If you use any other mail-order service to fill your prescription drugs, or you purchase them outside of the U.S., the plan will not cover these drugs if UMP is your primary plan. ALERT! When you use network pharmacies, retail or mail-order, you pay based on the prescription drug’s allowed amount, a discounted price negotiated with the plan. If you use a non-network pharmacy, the pharmacy may charge more than the allowed amount. You will have to pay this additional amount, which does not apply to your deductible or out-of-pocket limit. If you have other prescription drug coverage If you have primary medical coverage through another plan that covers prescription drugs, some of the limits and restrictions to prescription drug coverage listed on page 121 will apply when UMP pays secondary to another plan. See the “Submitting a claim for prescription drugs” section for how to submit your prescription drug claim. Using network pharmacies when UMP is secondary If you have primary coverage through another plan that covers prescription drugs, show both plan cards to the pharmacy and make sure they know which plan is primary. It is important that the pharmacy bills the plans in the correct order, or claims may be denied or paid incorrectly. 2024 UMP CDHP (PEBB) Certificate of Coverage 93
 UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 93 Page 95
UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 93 Page 95