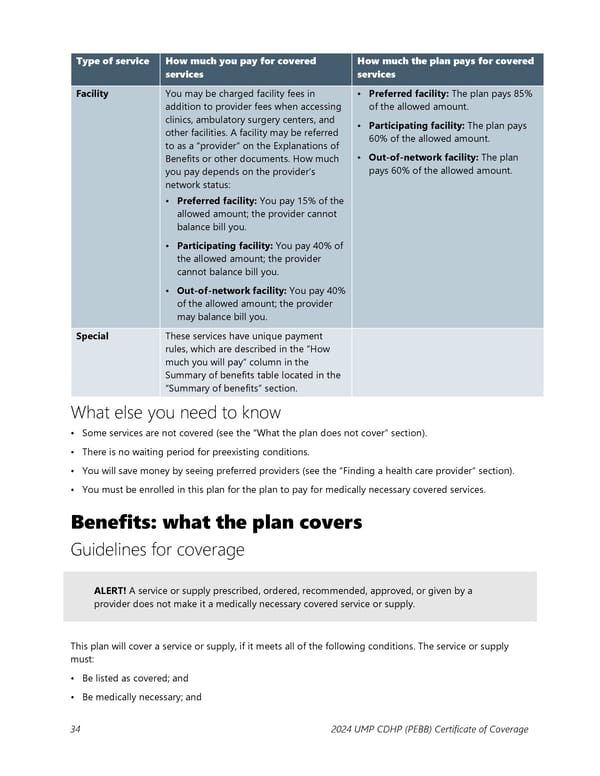
Type of service How much you pay for covered How much the plan pays for covered services services Facility You may be charged facility fees in • Preferred facility: The plan pays 85% addition to provider fees when accessing of the allowed amount. clinics, ambulatory surgery centers, and • Participating facility: The plan pays other facilities. A facility may be referred 60% of the allowed amount. to as a “provider” on the Explanations of • Out-of-network facility: The plan Benefits or other documents. How much pays 60% of the allowed amount. you pay depends on the provider’s network status: • Preferred facility: You pay 15% of the allowed amount; the provider cannot balance bill you. • Participating facility: You pay 40% of the allowed amount; the provider cannot balance bill you. • Out-of-network facility: You pay 40% of the allowed amount; the provider may balance bill you. Special These services have unique payment rules, which are described in the “How much you will pay” column in the Summary of benefits table located in the “Summary of benefits” section. What else you need to know • Some services are not covered (see the “What the plan does not cover” section). • There is no waiting period for preexisting conditions. • You will save money by seeing preferred providers (see the “Finding a health care provider” section). • You must be enrolled in this plan for the plan to pay for medically necessary covered services. Benefits: what the plan covers Guidelines for coverage ALERT! A service or supply prescribed, ordered, recommended, approved, or given by a provider does not make it a medically necessary covered service or supply. This plan will cover a service or supply, if it meets all of the following conditions. The service or supply must: • Be listed as covered; and • Be medically necessary; and 34 2024 UMP CDHP (PEBB) Certificate of Coverage
 UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 34 Page 36
UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 34 Page 36