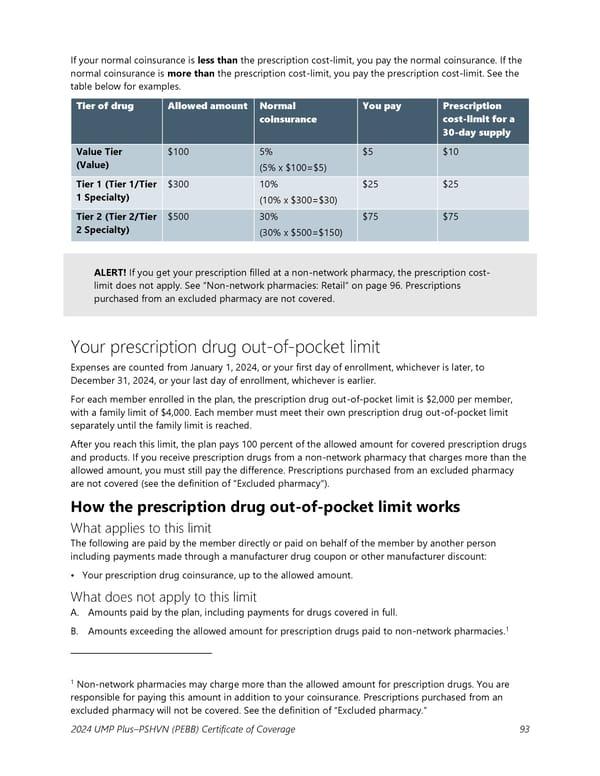
If your normal coinsurance is less than the prescription cost-limit, you pay the normal coinsurance. If the normal coinsurance is more than the prescription cost-limit, you pay the prescription cost-limit. See the table below for examples. Tier of drug Allowed amount Normal You pay Prescription coinsurance cost-limit for a 30-day supply Value Tier $100 5% $5 $10 (Value) (5% x $100=$5) Tier 1 (Tier 1/Tier $300 10% $25 $25 1 Specialty) (10% x $300=$30) Tier 2 (Tier 2/Tier $500 30% $75 $75 2 Specialty) (30% x $500=$150) ALERT! If you get your prescription filled at a non-network pharmacy, the prescription cost- limit does not apply. See “Non-network pharmacies: Retail” on page 96. Prescriptions purchased from an excluded pharmacy are not covered. Your prescription drug out-of-pocket limit Expenses are counted from January 1, 2024, or your first day of enrollment, whichever is later, to December 31, 2024, or your last day of enrollment, whichever is earlier. For each member enrolled in the plan, the prescription drug out-of-pocket limit is $2,000 per member, with a family limit of $4,000. Each member must meet their own prescription drug out-of-pocket limit separately until the family limit is reached. After you reach this limit, the plan pays 100 percent of the allowed amount for covered prescription drugs and products. If you receive prescription drugs from a non-network pharmacy that charges more than the allowed amount, you must still pay the difference. Prescriptions purchased from an excluded pharmacy are not covered (see the definition of “Excluded pharmacy”). How the prescription drug out-of-pocket limit works What applies to this limit The following are paid by the member directly or paid on behalf of the member by another person including payments made through a manufacturer drug coupon or other manufacturer discount: • Your prescription drug coinsurance, up to the allowed amount. What does not apply to this limit A. Amounts paid by the plan, including payments for drugs covered in full. 1 B. Amounts exceeding the allowed amount for prescription drugs paid to non-network pharmacies. 1 Non-network pharmacies may charge more than the allowed amount for prescription drugs. You are responsible for paying this amount in addition to your coinsurance. Prescriptions purchased from an excluded pharmacy will not be covered. See the definition of “Excluded pharmacy.” 2024 UMP Plus–PSHVN (PEBB) Certificate of Coverage 93
 UMP Plus–Puget Sound High Value Network (PSHVN) COC (2024) Page 93 Page 95
UMP Plus–Puget Sound High Value Network (PSHVN) COC (2024) Page 93 Page 95