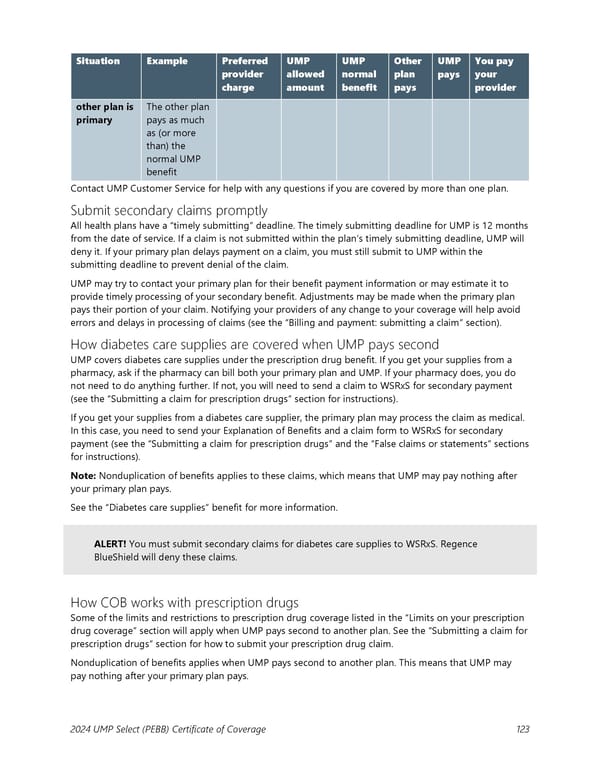
Situation Example Preferred UMP UMP Other UMP You pay provider allowed normal plan pays your charge amount benefit pays provider other plan is The other plan primary pays as much as (or more than) the normal UMP benefit Contact UMP Customer Service for help with any questions if you are covered by more than one plan. Submit secondary claims promptly All health plans have a “timely submitting” deadline. The timely submitting deadline for UMP is 12 months from the date of service. If a claim is not submitted within the plan’s timely submitting deadline, UMP will deny it. If your primary plan delays payment on a claim, you must still submit to UMP within the submitting deadline to prevent denial of the claim. UMP may try to contact your primary plan for their benefit payment information or may estimate it to provide timely processing of your secondary benefit. Adjustments may be made when the primary plan pays their portion of your claim. Notifying your providers of any change to your coverage will help avoid errors and delays in processing of claims (see the “Billing and payment: submitting a claim” section). How diabetes care supplies are covered when UMP pays second UMP covers diabetes care supplies under the prescription drug benefit. If you get your supplies from a pharmacy, ask if the pharmacy can bill both your primary plan and UMP. If your pharmacy does, you do not need to do anything further. If not, you will need to send a claim to WSRxS for secondary payment (see the “Submitting a claim for prescription drugs” section for instructions). If you get your supplies from a diabetes care supplier, the primary plan may process the claim as medical. In this case, you need to send your Explanation of Benefits and a claim form to WSRxS for secondary payment (see the “Submitting a claim for prescription drugs” and the “False claims or statements” sections for instructions). Note: Nonduplication of benefits applies to these claims, which means that UMP may pay nothing after your primary plan pays. See the “Diabetes care supplies” benefit for more information. ALERT! You must submit secondary claims for diabetes care supplies to WSRxS. Regence BlueShield will deny these claims. How COB works with prescription drugs Some of the limits and restrictions to prescription drug coverage listed in the “Limits on your prescription drug coverage” section will apply when UMP pays second to another plan. See the “Submitting a claim for prescription drugs” section for how to submit your prescription drug claim. Nonduplication of benefits applies when UMP pays second to another plan. This means that UMP may pay nothing after your primary plan pays. 2024 UMP Select (PEBB) Certificate of Coverage 123
 UMP Select COC (2024) Page 123 Page 125
UMP Select COC (2024) Page 123 Page 125