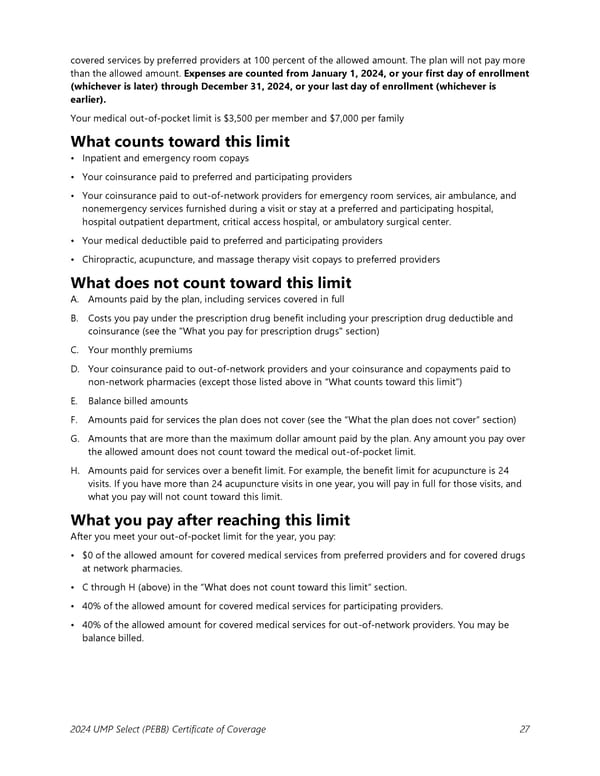
covered services by preferred providers at 100 percent of the allowed amount. The plan will not pay more than the allowed amount. Expenses are counted from January 1, 2024, or your first day of enrollment (whichever is later) through December 31, 2024, or your last day of enrollment (whichever is earlier). Your medical out-of-pocket limit is $3,500 per member and $7,000 per family What counts toward this limit • Inpatient and emergency room copays • Your coinsurance paid to preferred and participating providers • Your coinsurance paid to out-of-network providers for emergency room services, air ambulance, and nonemergency services furnished during a visit or stay at a preferred and participating hospital, hospital outpatient department, critical access hospital, or ambulatory surgical center. • Your medical deductible paid to preferred and participating providers • Chiropractic, acupuncture, and massage therapy visit copays to preferred providers What does not count toward this limit A. Amounts paid by the plan, including services covered in full B. Costs you pay under the prescription drug benefit including your prescription drug deductible and coinsurance (see the "What you pay for prescription drugs" section) C. Your monthly premiums D. Your coinsurance paid to out-of-network providers and your coinsurance and copayments paid to non-network pharmacies (except those listed above in “What counts toward this limit”) E. Balance billed amounts F. Amounts paid for services the plan does not cover (see the “What the plan does not cover” section) G. Amounts that are more than the maximum dollar amount paid by the plan. Any amount you pay over the allowed amount does not count toward the medical out-of-pocket limit. H. Amounts paid for services over a benefit limit. For example, the benefit limit for acupuncture is 24 visits. If you have more than 24 acupuncture visits in one year, you will pay in full for those visits, and what you pay will not count toward this limit. What you pay after reaching this limit After you meet your out-of-pocket limit for the year, you pay: • $0 of the allowed amount for covered medical services from preferred providers and for covered drugs at network pharmacies. • C through H (above) in the “What does not count toward this limit” section. • 40% of the allowed amount for covered medical services for participating providers. • 40% of the allowed amount for covered medical services for out-of-network providers. You may be balance billed. 2024 UMP Select (PEBB) Certificate of Coverage 27
 UMP Select COC (2024) Page 27 Page 29
UMP Select COC (2024) Page 27 Page 29