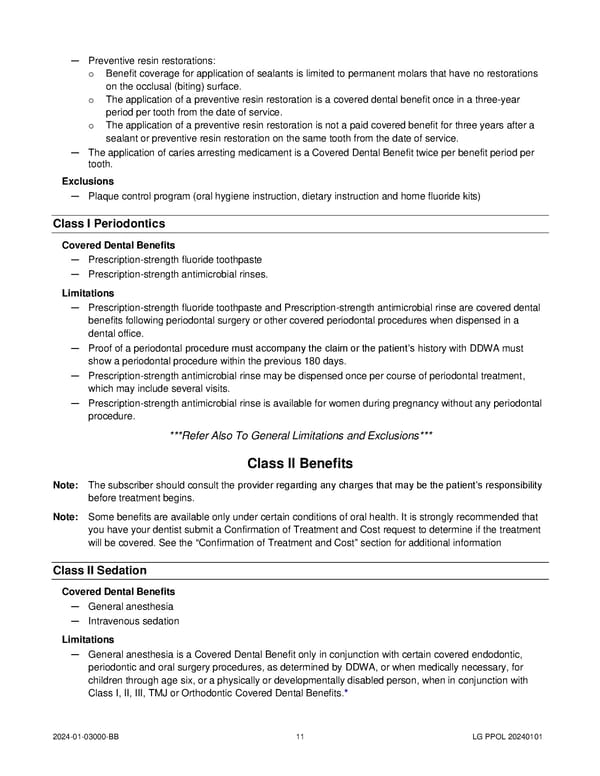
— Preventive resin restorations: o Benefit coverage for application of sealants is limited to permanent molars that have no restorations on the occlusal (biting) surface. o The application of a preventive resin restoration is a covered dental benefit once in a three-year period per tooth from the date of service. o The application of a preventive resin restoration is not a paid covered benefit for three years after a sealant or preventive resin restoration on the same tooth from the date of service. — The application of caries arresting medicament is a Covered Dental Benefit twice per benefit period per tooth. Exclusions — Plaque control program (oral hygiene instruction, dietary instruction and home fluoride kits) Class I Periodontics Covered Dental Benefits — Prescription-strength fluoride toothpaste — Prescription-strength antimicrobial rinses. Limitations — Prescription-strength fluoride toothpaste and Prescription-strength antimicrobial rinse are covered dental benefits following periodontal surgery or other covered periodontal procedures when dispensed in a dental office. — Proof of a periodontal procedure must accompany the claim or the patient’s history with DDWA must show a periodontal procedure within the previous 180 days. — Prescription-strength antimicrobial rinse may be dispensed once per course of periodontal treatment, which may include several visits. — Prescription-strength antimicrobial rinse is available for women during pregnancy without any periodontal procedure. ***Refer Also To General Limitations and Exclusions*** Class II Benefits Note: The subscriber should consult the provider regarding any charges that may be the patient’s responsibility before treatment begins. Note: Some benefits are available only under certain conditions of oral health. It is strongly recommended that you have your dentist submit a Confirmation of Treatment and Cost request to determine if the treatment will be covered. See the “Confirmation of Treatment and Cost” section for additional information Class II Sedation Covered Dental Benefits — General anesthesia — Intravenous sedation Limitations — General anesthesia is a Covered Dental Benefit only in conjunction with certain covered endodontic, periodontic and oral surgery procedures, as determined by DDWA, or when medically necessary, for children through age six, or a physically or developmentally disabled person, when in conjunction with Class I, II, III, TMJ or Orthodontic Covered Dental Benefits.* 2024-01-03000-BB 11 LG PPOL 20240101
 Uniform Dental Plan COC (2024) Page 15 Page 17
Uniform Dental Plan COC (2024) Page 15 Page 17