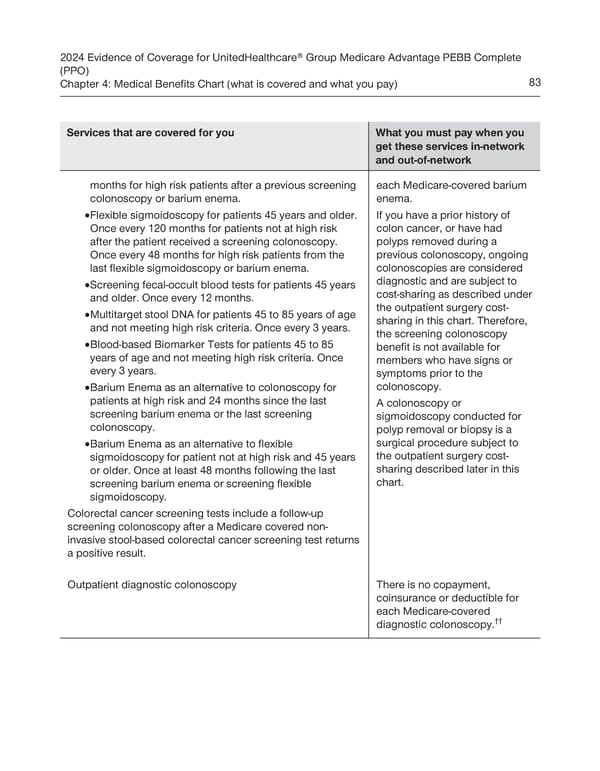
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Complete (PPO) Chapter 4: Medical Benefits Chart (what is covered and what you pay) 83 Services that are covered for you What you must pay when you get these services in-network and out-of-network months for high risk patients after a previous screening each Medicare-covered barium colonoscopy or barium enema. enema. · Flexible sigmoidoscopy for patients 45 years and older. If you have a prior history of Once every 120 months for patients not at high risk colon cancer, or have had after the patient received a screening colonoscopy. polyps removed during a Once every 48 months for high risk patients from the previous colonoscopy, ongoing last flexible sigmoidoscopy or barium enema. colonoscopies are considered · Screening fecal-occult blood tests for patients 45 years diagnostic and are subject to and older. Once every 12 months. cost-sharing as described under · Multitarget stool DNA for patients 45 to 85 years of age the outpatient surgery cost- and not meeting high risk criteria. Once every 3 years. sharing in this chart. Therefore, the screening colonoscopy · Blood-based Biomarker Tests for patients 45 to 85 benefit is not available for years of age and not meeting high risk criteria. Once members who have signs or every 3 years. symptoms prior to the · Barium Enema as an alternative to colonoscopy for colonoscopy. patients at high risk and 24 months since the last A colonoscopy or screening barium enema or the last screening sigmoidoscopy conducted for colonoscopy. polyp removal or biopsy is a · Barium Enema as an alternative to flexible surgical procedure subject to sigmoidoscopy for patient not at high risk and 45 years the outpatient surgery cost- or older. Once at least 48 months following the last sharing described later in this screening barium enema or screening flexible chart. sigmoidoscopy. Colorectal cancer screening tests include a follow-up screening colonoscopy after a Medicare covered non- invasive stool-based colorectal cancer screening test returns a positive result. Outpatient diagnostic colonoscopy There is no copayment, coinsurance or deductible for each Medicare-covered diagnostic colonoscopy.††
 UnitedHealthcare PEBB Complete EOC (2024) Page 88 Page 90
UnitedHealthcare PEBB Complete EOC (2024) Page 88 Page 90