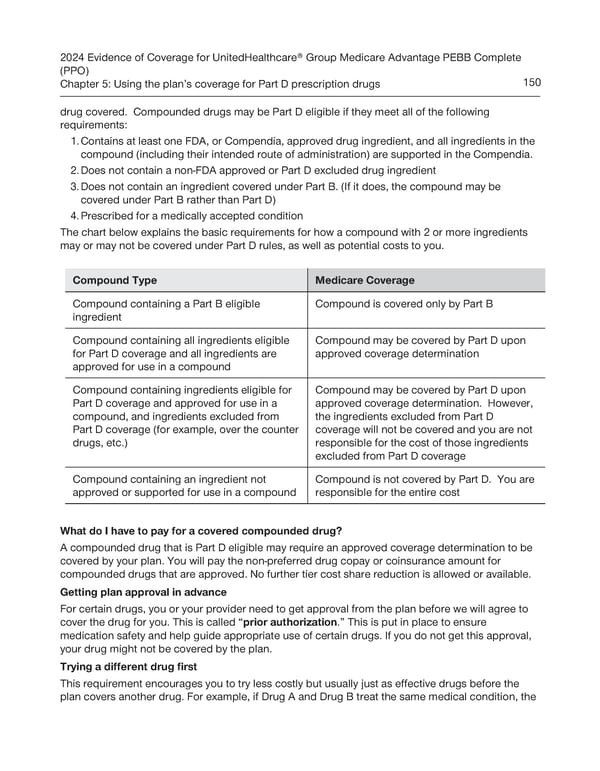
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Complete (PPO) Chapter 5: Using the plan’s coverage for Part D prescription drugs 150 drug covered. Compounded drugs may be Part D eligible if they meet all of the following requirements: 1. Contains at least one FDA, or Compendia, approved drug ingredient, and all ingredients in the compound (including their intended route of administration) are supported in the Compendia. 2. Does not contain a non-FDA approved or Part D excluded drug ingredient 3. Does not contain an ingredient covered under Part B. (If it does, the compound may be covered under Part B rather than Part D) 4. Prescribed for a medically accepted condition The chart below explains the basic requirements for how a compound with 2 or more ingredients may or may not be covered under Part D rules, as well as potential costs to you. Compound Type Medicare Coverage Compound containing a Part B eligible Compound is covered only by Part B ingredient Compound containing all ingredients eligible Compound may be covered by Part D upon for Part D coverage and all ingredients are approved coverage determination approved for use in a compound Compound containing ingredients eligible for Compound may be covered by Part D upon Part D coverage and approved for use in a approved coverage determination. However, compound, and ingredients excluded from the ingredients excluded from Part D Part D coverage (for example, over the counter coverage will not be covered and you are not drugs, etc.) responsible for the cost of those ingredients excluded from Part D coverage Compound containing an ingredient not Compound is not covered by Part D. You are approved or supported for use in a compound responsible for the entire cost What do I have to pay for a covered compounded drug? A compounded drug that is Part D eligible may require an approved coverage determination to be covered by your plan. You will pay the non-preferred drug copay or coinsurance amount for compounded drugs that are approved. No further tier cost share reduction is allowed or available. Getting plan approval in advance For certain drugs, you or your provider need to get approval from the plan before we will agree to cover the drug for you. This is called “prior authorization.” This is put in place to ensure medication safety and help guide appropriate use of certain drugs. If you do not get this approval, your drug might not be covered by the plan. Trying a different drug first This requirement encourages you to try less costly but usually just as effective drugs before the plan covers another drug. For example, if Drug A and Drug B treat the same medical condition, the
 UnitedHealthcare PEBB Complete EOC (2024) Page 155 Page 157
UnitedHealthcare PEBB Complete EOC (2024) Page 155 Page 157