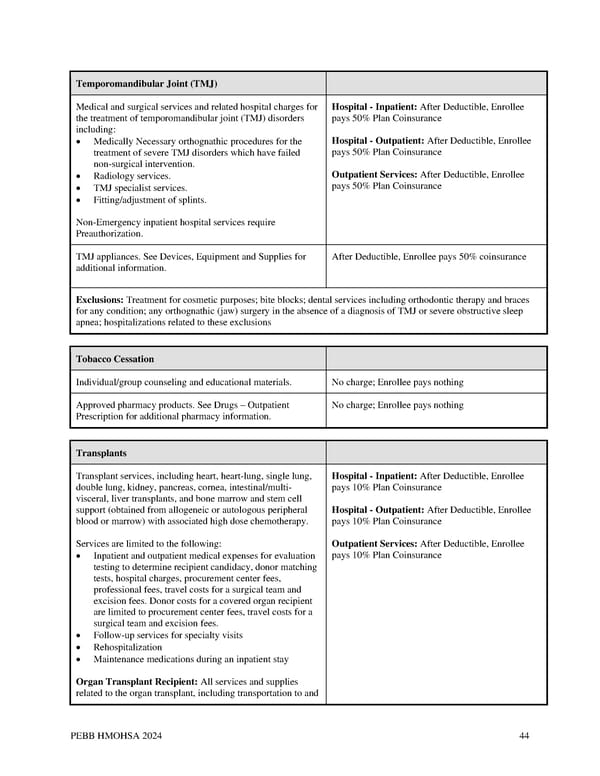
Temporomandibular Joint (TMJ) Medical and surgical services and related hospital charges for Hospital - Inpatient: After Deductible, Enrollee the treatment of temporomandibular joint (TMJ) disorders pays 50% Plan Coinsurance including: • Medically Necessary orthognathic procedures for the Hospital - Outpatient: After Deductible, Enrollee treatment of severe TMJ disorders which have failed pays 50% Plan Coinsurance non-surgical intervention. • Radiology services. Outpatient Services: After Deductible, Enrollee • TMJ specialist services. pays 50% Plan Coinsurance • Fitting/adjustment of splints. Non-Emergency inpatient hospital services require Preauthorization. TMJ appliances. See Devices, Equipment and Supplies for After Deductible, Enrollee pays 50% coinsurance additional information. Exclusions: Treatment for cosmetic purposes; bite blocks; dental services including orthodontic therapy and braces for any condition; any orthognathic (jaw) surgery in the absence of a diagnosis of TMJ or severe obstructive sleep apnea; hospitalizations related to these exclusions Tobacco Cessation Individual/group counseling and educational materials. No charge; Enrollee pays nothing Approved pharmacy products. See Drugs – Outpatient No charge; Enrollee pays nothing Prescription for additional pharmacy information. Transplants Transplant services, including heart, heart-lung, single lung, Hospital - Inpatient: After Deductible, Enrollee double lung, kidney, pancreas, cornea, intestinal/multi- pays 10% Plan Coinsurance visceral, liver transplants, and bone marrow and stem cell support (obtained from allogeneic or autologous peripheral Hospital - Outpatient: After Deductible, Enrollee blood or marrow) with associated high dose chemotherapy. pays 10% Plan Coinsurance Services are limited to the following: Outpatient Services: After Deductible, Enrollee • Inpatient and outpatient medical expenses for evaluation pays 10% Plan Coinsurance testing to determine recipient candidacy, donor matching tests, hospital charges, procurement center fees, professional fees, travel costs for a surgical team and excision fees. Donor costs for a covered organ recipient are limited to procurement center fees, travel costs for a surgical team and excision fees. • Follow-up services for specialty visits • Rehospitalization • Maintenance medications during an inpatient stay Organ Transplant Recipient: All services and supplies related to the organ transplant, including transportation to and PEBB HMOHSA 2024 44
 Kaiser Permanente WA CDHP EOC (2024) Page 43 Page 45
Kaiser Permanente WA CDHP EOC (2024) Page 43 Page 45