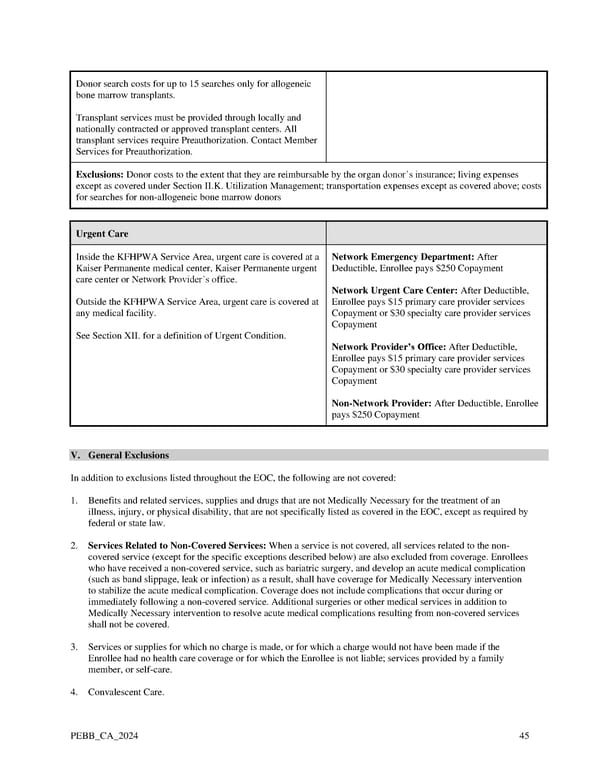
Donor search costs for up to 15 searches only for allogeneic bone marrow transplants. Transplant services must be provided through locally and nationally contracted or approved transplant centers. All transplant services require Preauthorization. Contact Member Services for Preauthorization. Exclusions: Donor costs to the extent that they are reimbursable by the organ donor’s insurance; living expenses except as covered under Section II.K. Utilization Management; transportation expenses except as covered above; costs for searches for non-allogeneic bone marrow donors Urgent Care Inside the KFHPWA Service Area, urgent care is covered at a Network Emergency Department: After Kaiser Permanente medical center, Kaiser Permanente urgent Deductible, Enrollee pays $250 Copayment care center or Network Provider’s office. Network Urgent Care Center: After Deductible, Outside the KFHPWA Service Area, urgent care is covered at Enrollee pays $15 primary care provider services any medical facility. Copayment or $30 specialty care provider services Copayment See Section XII. for a definition of Urgent Condition. Network Provider’s Office: After Deductible, Enrollee pays $15 primary care provider services Copayment or $30 specialty care provider services Copayment Non-Network Provider: After Deductible, Enrollee pays $250 Copayment V. General Exclusions In addition to exclusions listed throughout the EOC, the following are not covered: 1. Benefits and related services, supplies and drugs that are not Medically Necessary for the treatment of an illness, injury, or physical disability, that are not specifically listed as covered in the EOC, except as required by federal or state law. 2. Services Related to Non-Covered Services: When a service is not covered, all services related to the non- covered service (except for the specific exceptions described below) are also excluded from coverage. Enrollees who have received a non-covered service, such as bariatric surgery, and develop an acute medical complication (such as band slippage, leak or infection) as a result, shall have coverage for Medically Necessary intervention to stabilize the acute medical complication. Coverage does not include complications that occur during or immediately following a non-covered service. Additional surgeries or other medical services in addition to Medically Necessary intervention to resolve acute medical complications resulting from non-covered services shall not be covered. 3. Services or supplies for which no charge is made, or for which a charge would not have been made if the Enrollee had no health care coverage or for which the Enrollee is not liable; services provided by a family member, or self-care. 4. Convalescent Care. PEBB_CA_2024 45
 Kaiser Permanente WA Classic EOC (2024) Page 44 Page 46
Kaiser Permanente WA Classic EOC (2024) Page 44 Page 46