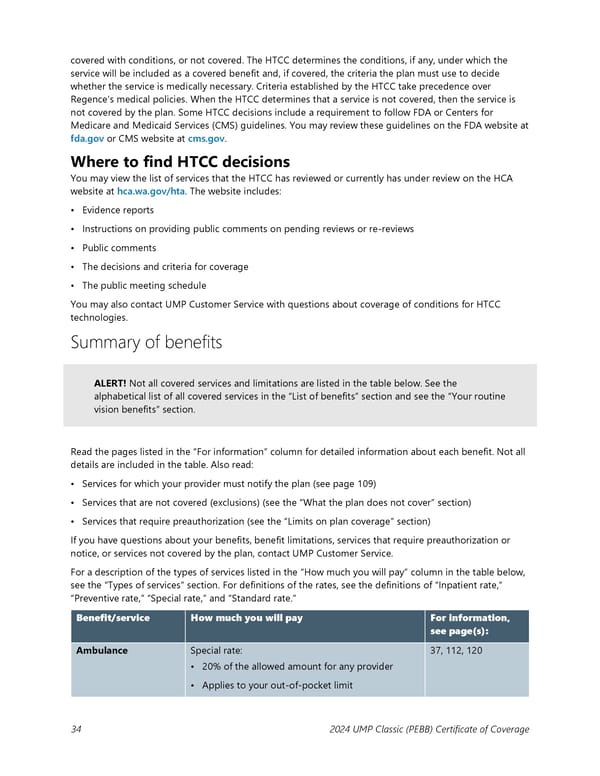
covered with conditions, or not covered. The HTCC determines the conditions, if any, under which the service will be included as a covered benefit and, if covered, the criteria the plan must use to decide whether the service is medically necessary. Criteria established by the HTCC take precedence over Regence’s medical policies. When the HTCC determines that a service is not covered, then the service is not covered by the plan. Some HTCC decisions include a requirement to follow FDA or Centers for Medicare and Medicaid Services (CMS) guidelines. You may review these guidelines on the FDA website at fda.gov or CMS website at cms.gov. Where to find HTCC decisions You may view the list of services that the HTCC has reviewed or currently has under review on the HCA website at hca.wa.gov/hta. The website includes: • Evidence reports • Instructions on providing public comments on pending reviews or re-reviews • Public comments • The decisions and criteria for coverage • The public meeting schedule You may also contact UMP Customer Service with questions about coverage of conditions for HTCC technologies. Summary of benefits ALERT! Not all covered services and limitations are listed in the table below. See the alphabetical list of all covered services in the “List of benefits” section and see the “Your routine vision benefits” section. Read the pages listed in the “For information” column for detailed information about each benefit. Not all details are included in the table. Also read: • Services for which your provider must notify the plan (see page 109) • Services that are not covered (exclusions) (see the “What the plan does not cover” section) • Services that require preauthorization (see the “Limits on plan coverage” section) If you have questions about your benefits, benefit limitations, services that require preauthorization or notice, or services not covered by the plan, contact UMP Customer Service. For a description of the types of services listed in the “How much you will pay” column in the table below, see the “Types of services” section. For definitions of the rates, see the definitions of “Inpatient rate,” “Preventive rate,” “Special rate,” and “Standard rate.” Benefit/service How much you will pay For information, see page(s): Ambulance Special rate: 37, 112, 120 • 20% of the allowed amount for any provider • Applies to your out-of-pocket limit 34 2024 UMP Classic (PEBB) Certificate of Coverage
 UMP Classic COC (2024) Page 34 Page 36
UMP Classic COC (2024) Page 34 Page 36