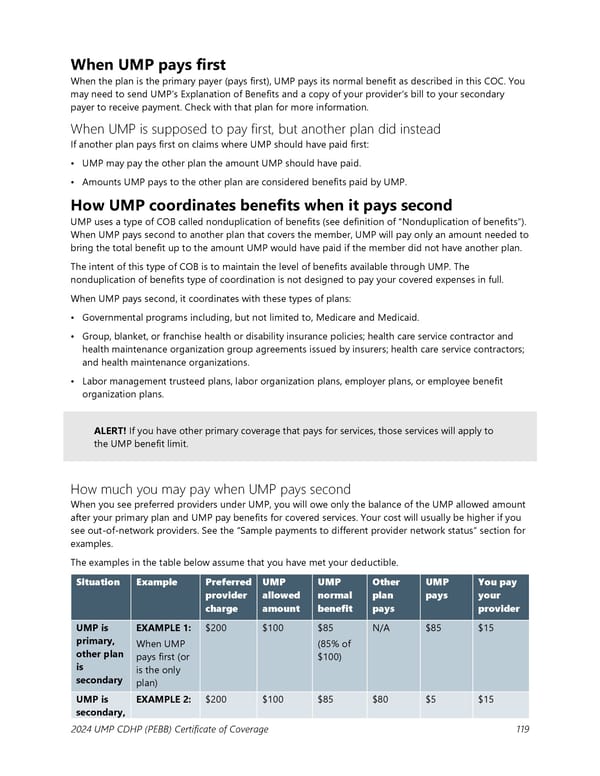
When UMP pays first When the plan is the primary payer (pays first), UMP pays its normal benefit as described in this COC. You may need to send UMP’s Explanation of Benefits and a copy of your provider’s bill to your secondary payer to receive payment. Check with that plan for more information. When UMP is supposed to pay first, but another plan did instead If another plan pays first on claims where UMP should have paid first: • UMP may pay the other plan the amount UMP should have paid. • Amounts UMP pays to the other plan are considered benefits paid by UMP. How UMP coordinates benefits when it pays second UMP uses a type of COB called nonduplication of benefits (see definition of “Nonduplication of benefits”). When UMP pays second to another plan that covers the member, UMP will pay only an amount needed to bring the total benefit up to the amount UMP would have paid if the member did not have another plan. The intent of this type of COB is to maintain the level of benefits available through UMP. The nonduplication of benefits type of coordination is not designed to pay your covered expenses in full. When UMP pays second, it coordinates with these types of plans: • Governmental programs including, but not limited to, Medicare and Medicaid. • Group, blanket, or franchise health or disability insurance policies; health care service contractor and health maintenance organization group agreements issued by insurers; health care service contractors; and health maintenance organizations. • Labor management trusteed plans, labor organization plans, employer plans, or employee benefit organization plans. ALERT! If you have other primary coverage that pays for services, those services will apply to the UMP benefit limit. How much you may pay when UMP pays second When you see preferred providers under UMP, you will owe only the balance of the UMP allowed amount after your primary plan and UMP pay benefits for covered services. Your cost will usually be higher if you see out-of-network providers. See the “Sample payments to different provider network status” section for examples. The examples in the table below assume that you have met your deductible. Situation Example Preferred UMP UMP Other UMP You pay provider allowed normal plan pays your charge amount benefit pays provider UMP is EXAMPLE 1: $200 $100 $85 N/A $85 $15 primary, When UMP (85% of other plan pays first (or $100) is is the only secondary plan) UMP is EXAMPLE 2: $200 $100 $85 $80 $5 $15 secondary, 2024 UMP CDHP (PEBB) Certificate of Coverage 119
 UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 119 Page 121
UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 119 Page 121