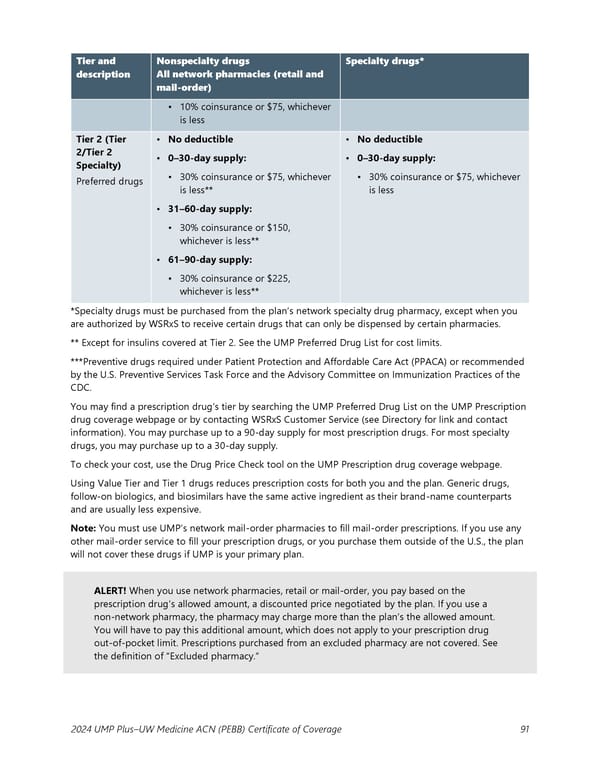
Tier and Nonspecialty drugs Specialty drugs* description All network pharmacies (retail and mail-order) ▪ 10% coinsurance or $75, whichever is less Tier 2 (Tier • No deductible • No deductible 2/Tier 2 • 0–30-day supply: • 0–30-day supply: Specialty) ▪ 30% coinsurance or $75, whichever ▪ 30% coinsurance or $75, whichever Preferred drugs is less** is less • 31–60-day supply: ▪ 30% coinsurance or $150, whichever is less** • 61–90-day supply: ▪ 30% coinsurance or $225, whichever is less** *Specialty drugs must be purchased from the plan’s network specialty drug pharmacy, except when you are authorized by WSRxS to receive certain drugs that can only be dispensed by certain pharmacies. ** Except for insulins covered at Tier 2. See the UMP Preferred Drug List for cost limits. ***Preventive drugs required under Patient Protection and Affordable Care Act (PPACA) or recommended by the U.S. Preventive Services Task Force and the Advisory Committee on Immunization Practices of the CDC. You may find a prescription drug’s tier by searching the UMP Preferred Drug List on the UMP Prescription drug coverage webpage or by contacting WSRxS Customer Service (see Directory for link and contact information). You may purchase up to a 90-day supply for most prescription drugs. For most specialty drugs, you may purchase up to a 30-day supply. To check your cost, use the Drug Price Check tool on the UMP Prescription drug coverage webpage. Using Value Tier and Tier 1 drugs reduces prescription costs for both you and the plan. Generic drugs, follow-on biologics, and biosimilars have the same active ingredient as their brand-name counterparts and are usually less expensive. Note: You must use UMP’s network mail-order pharmacies to fill mail-order prescriptions. If you use any other mail-order service to fill your prescription drugs, or you purchase them outside of the U.S., the plan will not cover these drugs if UMP is your primary plan. ALERT! When you use network pharmacies, retail or mail-order, you pay based on the prescription drug’s allowed amount, a discounted price negotiated by the plan. If you use a non-network pharmacy, the pharmacy may charge more than the plan’s the allowed amount. You will have to pay this additional amount, which does not apply to your prescription drug out-of-pocket limit. Prescriptions purchased from an excluded pharmacy are not covered. See the definition of “Excluded pharmacy.” 2024 UMP Plus–UW Medicine ACN (PEBB) Certificate of Coverage 91
 UMP Plus–UW Medicine Accountable Care Network (UW Medicine ACN) COC (2024) Page 91 Page 93
UMP Plus–UW Medicine Accountable Care Network (UW Medicine ACN) COC (2024) Page 91 Page 93