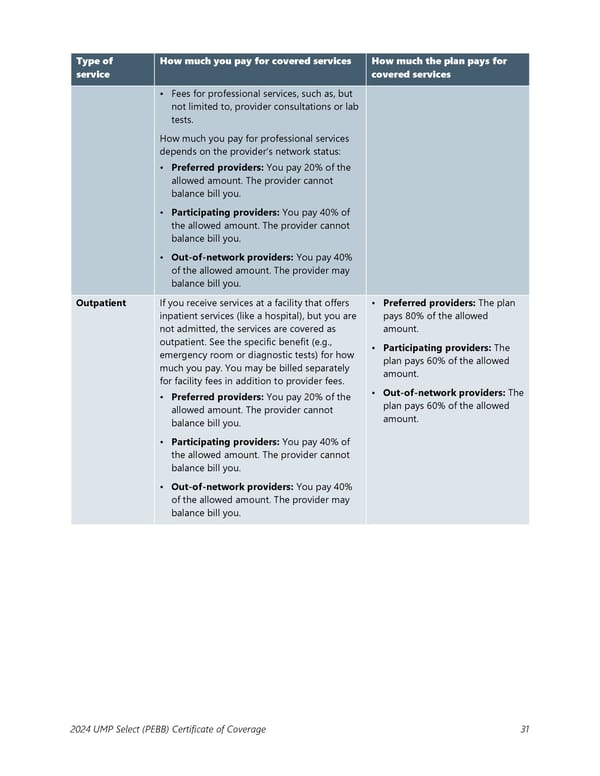
Type of How much you pay for covered services How much the plan pays for service covered services • Fees for professional services, such as, but not limited to, provider consultations or lab tests. How much you pay for professional services depends on the provider’s network status: • Preferred providers: You pay 20% of the allowed amount. The provider cannot balance bill you. • Participating providers: You pay 40% of the allowed amount. The provider cannot balance bill you. • Out-of-network providers: You pay 40% of the allowed amount. The provider may balance bill you. Outpatient If you receive services at a facility that offers • Preferred providers: The plan inpatient services (like a hospital), but you are pays 80% of the allowed not admitted, the services are covered as amount. outpatient. See the specific benefit (e.g., • Participating providers: The emergency room or diagnostic tests) for how plan pays 60% of the allowed much you pay. You may be billed separately amount. for facility fees in addition to provider fees. • Out-of-network providers: The • Preferred providers: You pay 20% of the plan pays 60% of the allowed allowed amount. The provider cannot amount. balance bill you. • Participating providers: You pay 40% of the allowed amount. The provider cannot balance bill you. • Out-of-network providers: You pay 40% of the allowed amount. The provider may balance bill you. 2024 UMP Select (PEBB) Certificate of Coverage 31
 UMP Select COC (2024) Page 31 Page 33
UMP Select COC (2024) Page 31 Page 33