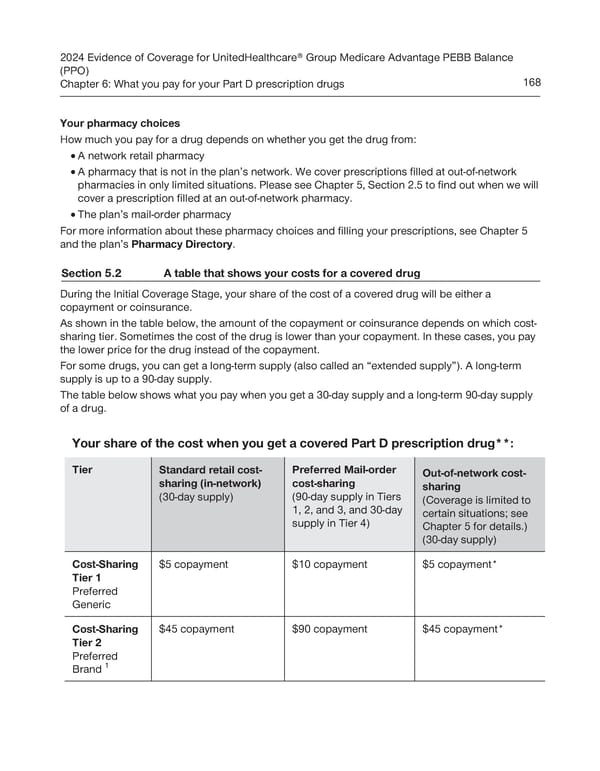
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Balance (PPO) Chapter 6: What you pay for your Part D prescription drugs 168 Your pharmacy choices How much you pay for a drug depends on whether you get the drug from: A network retail pharmacy · · A pharmacy that is not in the plan’s network. We cover prescriptions filled at out-of-network pharmacies in only limited situations. Please see Chapter 5, Section 2.5 to find out when we will cover a prescription filled at an out-of-network pharmacy. · The plan’s mail-order pharmacy For more information about these pharmacy choices and filling your prescriptions, see Chapter 5 and the plan’s Pharmacy Directory. Section 5.2 A table that shows your costs for a covered drug During the Initial Coverage Stage, your share of the cost of a covered drug will be either a copayment or coinsurance. As shown in the table below, the amount of the copayment or coinsurance depends on which cost- sharing tier. Sometimes the cost of the drug is lower than your copayment. In these cases, you pay the lower price for the drug instead of the copayment. For some drugs, you can get a long-term supply (also called an “extended supply”). A long-term supply is up to a 90-day supply. The table below shows what you pay when you get a 30-day supply and a long-term 90-day supply of a drug. Your share of the cost when you get a covered Part D prescription drug**: Tier Standard retail cost- Preferred Mail-order Out-of-network cost- sharing (in-network) cost-sharing sharing (30-day supply) (90-day supply in Tiers (Coverage is limited to 1, 2, and 3, and 30-day certain situations; see supply in Tier 4) Chapter 5 for details.) (30-day supply) Cost-Sharing $5 copayment $10 copayment $5 copayment* Tier 1 Preferred Generic Cost-Sharing $45 copayment $90 copayment $45 copayment* Tier 2 Preferred 1 Brand
 UnitedHealthcare PEBB Balance EOC (2024) Page 173 Page 175
UnitedHealthcare PEBB Balance EOC (2024) Page 173 Page 175