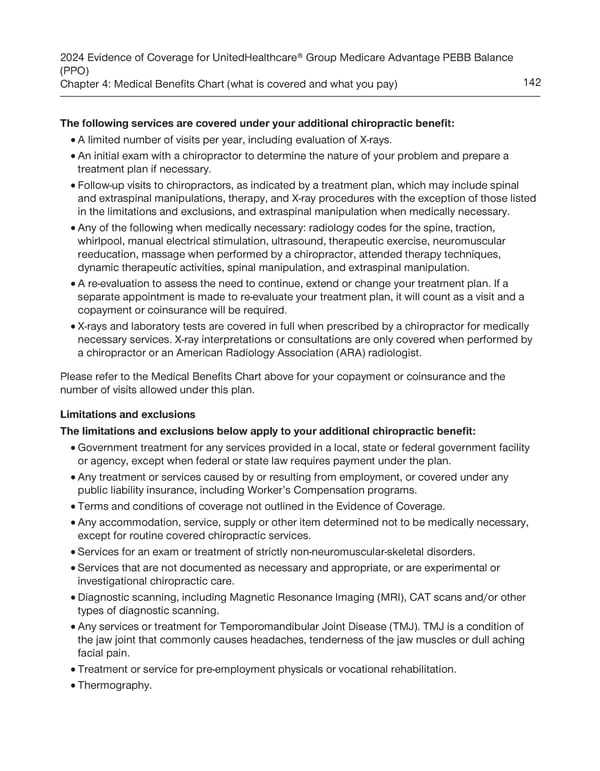
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Balance (PPO) Chapter 4: Medical Benefits Chart (what is covered and what you pay) 142 The following services are covered under your additional chiropractic benefit: · A limited number of visits per year, including evaluation of X-rays. · An initial exam with a chiropractor to determine the nature of your problem and prepare a treatment plan if necessary. · Follow-up visits to chiropractors, as indicated by a treatment plan, which may include spinal and extraspinal manipulations, therapy, and X-ray procedures with the exception of those listed in the limitations and exclusions, and extraspinal manipulation when medically necessary. · Any of the following when medically necessary: radiology codes for the spine, traction, whirlpool, manual electrical stimulation, ultrasound, therapeutic exercise, neuromuscular reeducation, massage when performed by a chiropractor, attended therapy techniques, dynamic therapeutic activities, spinal manipulation, and extraspinal manipulation. · A re-evaluation to assess the need to continue, extend or change your treatment plan. If a separate appointment is made to re-evaluate your treatment plan, it will count as a visit and a copayment or coinsurance will be required. · X-rays and laboratory tests are covered in full when prescribed by a chiropractor for medically necessary services. X-ray interpretations or consultations are only covered when performed by a chiropractor or an American Radiology Association (ARA) radiologist. Please refer to the Medical Benefits Chart above for your copayment or coinsurance and the number of visits allowed under this plan. Limitations and exclusions The limitations and exclusions below apply to your additional chiropractic benefit: · Government treatment for any services provided in a local, state or federal government facility or agency, except when federal or state law requires payment under the plan. · Any treatment or services caused by or resulting from employment, or covered under any public liability insurance, including Worker’s Compensation programs. · Terms and conditions of coverage not outlined in the Evidence of Coverage. · Any accommodation, service, supply or other item determined not to be medically necessary, except for routine covered chiropractic services. · Services for an exam or treatment of strictly non-neuromuscular-skeletal disorders. · Services that are not documented as necessary and appropriate, or are experimental or investigational chiropractic care. · Diagnostic scanning, including Magnetic Resonance Imaging (MRI), CAT scans and/or other types of diagnostic scanning. · Any services or treatment for Temporomandibular Joint Disease (TMJ). TMJ is a condition of the jaw joint that commonly causes headaches, tenderness of the jaw muscles or dull aching facial pain. Treatment or service for pre-employment physicals or vocational rehabilitation. · · Thermography.
 UnitedHealthcare PEBB Balance EOC (2024) Page 147 Page 149
UnitedHealthcare PEBB Balance EOC (2024) Page 147 Page 149