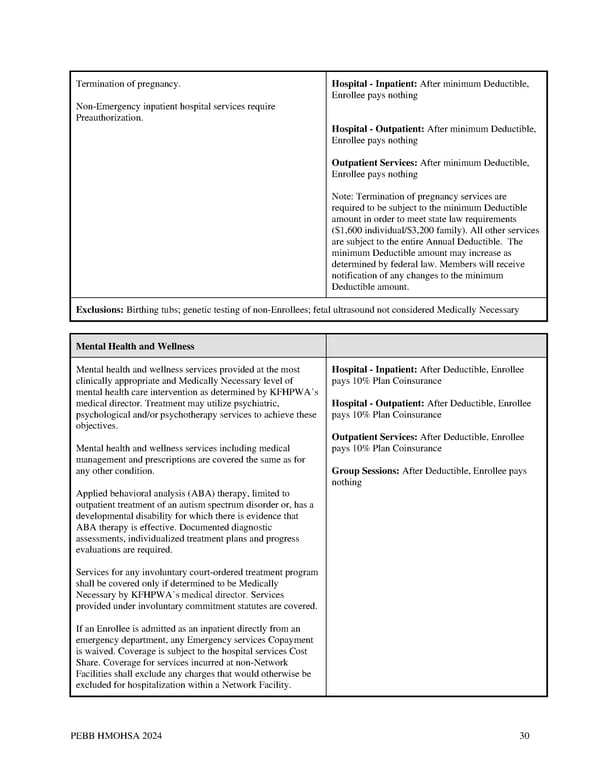
Termination of pregnancy. Hospital - Inpatient: After minimum Deductible, Enrollee pays nothing Non-Emergency inpatient hospital services require Preauthorization. Hospital - Outpatient: After minimum Deductible, Enrollee pays nothing Outpatient Services: After minimum Deductible, Enrollee pays nothing Note: Termination of pregnancy services are required to be subject to the minimum Deductible amount in order to meet state law requirements ($1,600 individual/$3,200 family). All other services are subject to the entire Annual Deductible. The minimum Deductible amount may increase as determined by federal law. Members will receive notification of any changes to the minimum Deductible amount. Exclusions: Birthing tubs; genetic testing of non-Enrollees; fetal ultrasound not considered Medically Necessary Mental Health and Wellness Mental health and wellness services provided at the most Hospital - Inpatient: After Deductible, Enrollee clinically appropriate and Medically Necessary level of pays 10% Plan Coinsurance mental health care intervention as determined by KFHPWA’s medical director. Treatment may utilize psychiatric, Hospital - Outpatient: After Deductible, Enrollee psychological and/or psychotherapy services to achieve these pays 10% Plan Coinsurance objectives. Outpatient Services: After Deductible, Enrollee Mental health and wellness services including medical pays 10% Plan Coinsurance management and prescriptions are covered the same as for any other condition. Group Sessions: After Deductible, Enrollee pays nothing Applied behavioral analysis (ABA) therapy, limited to outpatient treatment of an autism spectrum disorder or, has a developmental disability for which there is evidence that ABA therapy is effective. Documented diagnostic assessments, individualized treatment plans and progress evaluations are required. Services for any involuntary court-ordered treatment program shall be covered only if determined to be Medically Necessary by KFHPWA’s medical director. Services provided under involuntary commitment statutes are covered. If an Enrollee is admitted as an inpatient directly from an emergency department, any Emergency services Copayment is waived. Coverage is subject to the hospital services Cost Share. Coverage for services incurred at non-Network Facilities shall exclude any charges that would otherwise be excluded for hospitalization within a Network Facility. PEBB HMOHSA 2024 30
 Kaiser Permanente WA CDHP EOC (2024) Page 29 Page 31
Kaiser Permanente WA CDHP EOC (2024) Page 29 Page 31