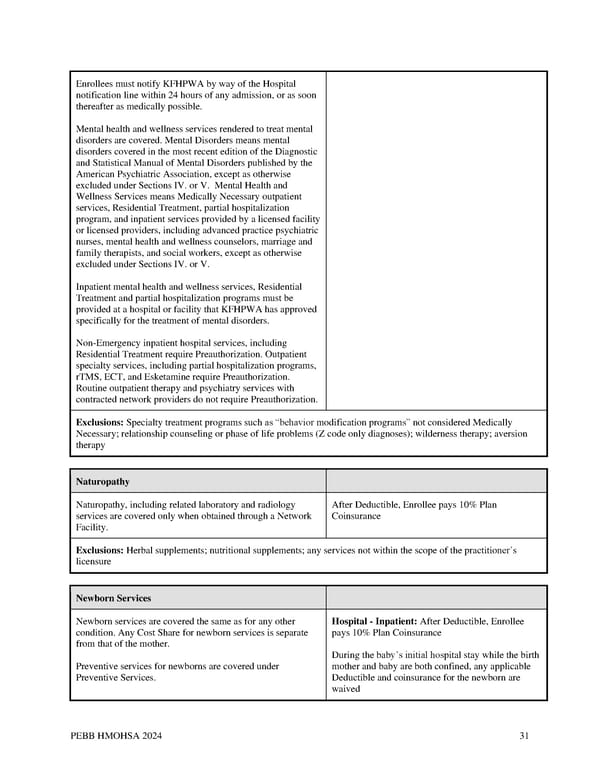
Enrollees must notify KFHPWA by way of the Hospital notification line within 24 hours of any admission, or as soon thereafter as medically possible. Mental health and wellness services rendered to treat mental disorders are covered. Mental Disorders means mental disorders covered in the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders published by the American Psychiatric Association, except as otherwise excluded under Sections IV. or V. Mental Health and Wellness Services means Medically Necessary outpatient services, Residential Treatment, partial hospitalization program, and inpatient services provided by a licensed facility or licensed providers, including advanced practice psychiatric nurses, mental health and wellness counselors, marriage and family therapists, and social workers, except as otherwise excluded under Sections IV. or V. Inpatient mental health and wellness services, Residential Treatment and partial hospitalization programs must be provided at a hospital or facility that KFHPWA has approved specifically for the treatment of mental disorders. Non-Emergency inpatient hospital services, including Residential Treatment require Preauthorization. Outpatient specialty services, including partial hospitalization programs, rTMS, ECT, and Esketamine require Preauthorization. Routine outpatient therapy and psychiatry services with contracted network providers do not require Preauthorization. Exclusions: Specialty treatment programs such as “behavior modification programs” not considered Medically Necessary; relationship counseling or phase of life problems (Z code only diagnoses); wilderness therapy; aversion therapy Naturopathy Naturopathy, including related laboratory and radiology After Deductible, Enrollee pays 10% Plan services are covered only when obtained through a Network Coinsurance Facility. Exclusions: Herbal supplements; nutritional supplements; any services not within the scope of the practitioner’s licensure Newborn Services Newborn services are covered the same as for any other Hospital - Inpatient: After Deductible, Enrollee condition. Any Cost Share for newborn services is separate pays 10% Plan Coinsurance from that of the mother. During the baby’s initial hospital stay while the birth Preventive services for newborns are covered under mother and baby are both confined, any applicable Preventive Services. Deductible and coinsurance for the newborn are waived PEBB HMOHSA 2024 31
 Kaiser Permanente WA CDHP EOC (2024) Page 30 Page 32
Kaiser Permanente WA CDHP EOC (2024) Page 30 Page 32