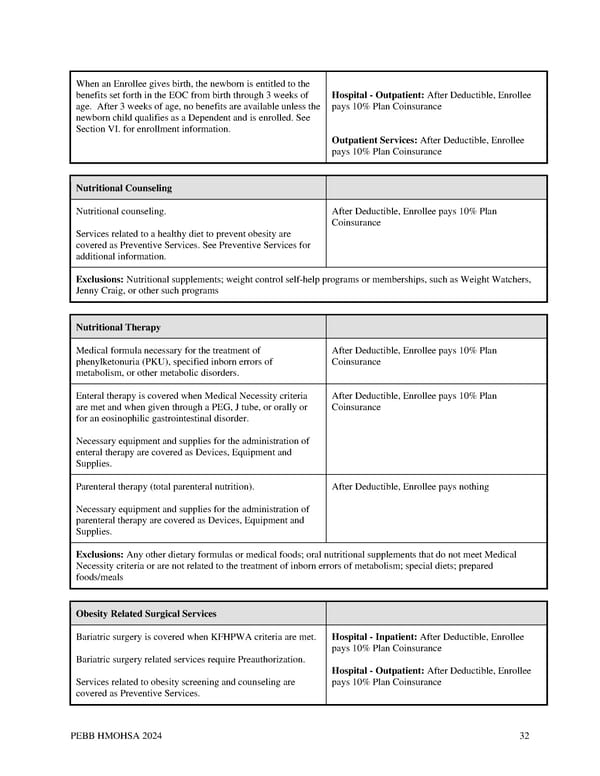
When an Enrollee gives birth, the newborn is entitled to the benefits set forth in the EOC from birth through 3 weeks of Hospital - Outpatient: After Deductible, Enrollee age. After 3 weeks of age, no benefits are available unless the pays 10% Plan Coinsurance newborn child qualifies as a Dependent and is enrolled. See Section VI. for enrollment information. Outpatient Services: After Deductible, Enrollee pays 10% Plan Coinsurance Nutritional Counseling Nutritional counseling. After Deductible, Enrollee pays 10% Plan Coinsurance Services related to a healthy diet to prevent obesity are covered as Preventive Services. See Preventive Services for additional information. Exclusions: Nutritional supplements; weight control self-help programs or memberships, such as Weight Watchers, Jenny Craig, or other such programs Nutritional Therapy Medical formula necessary for the treatment of After Deductible, Enrollee pays 10% Plan phenylketonuria (PKU), specified inborn errors of Coinsurance metabolism, or other metabolic disorders. Enteral therapy is covered when Medical Necessity criteria After Deductible, Enrollee pays 10% Plan are met and when given through a PEG, J tube, or orally or Coinsurance for an eosinophilic gastrointestinal disorder. Necessary equipment and supplies for the administration of enteral therapy are covered as Devices, Equipment and Supplies. Parenteral therapy (total parenteral nutrition). After Deductible, Enrollee pays nothing Necessary equipment and supplies for the administration of parenteral therapy are covered as Devices, Equipment and Supplies. Exclusions: Any other dietary formulas or medical foods; oral nutritional supplements that do not meet Medical Necessity criteria or are not related to the treatment of inborn errors of metabolism; special diets; prepared foods/meals Obesity Related Surgical Services Bariatric surgery is covered when KFHPWA criteria are met. Hospital - Inpatient: After Deductible, Enrollee pays 10% Plan Coinsurance Bariatric surgery related services require Preauthorization. Hospital - Outpatient: After Deductible, Enrollee Services related to obesity screening and counseling are pays 10% Plan Coinsurance covered as Preventive Services. PEBB HMOHSA 2024 32
 Kaiser Permanente WA CDHP EOC (2024) Page 31 Page 33
Kaiser Permanente WA CDHP EOC (2024) Page 31 Page 33