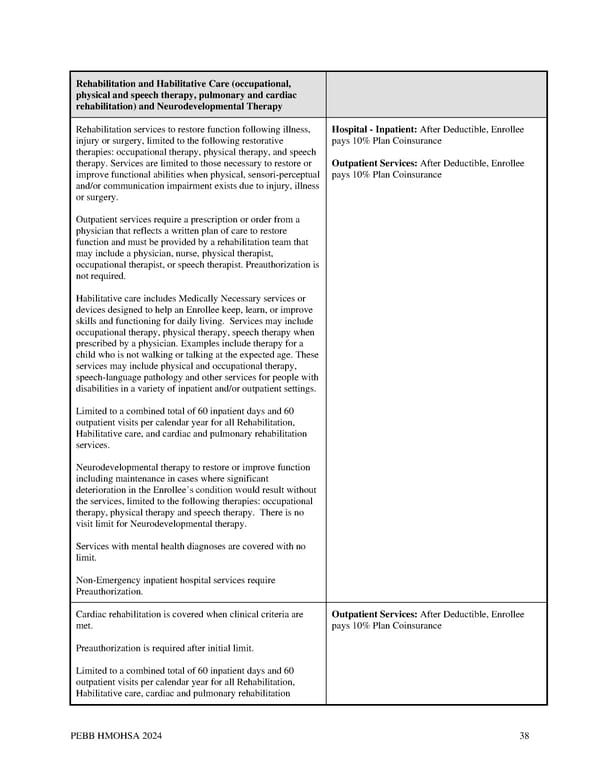
Rehabilitation and Habilitative Care (occupational, physical and speech therapy, pulmonary and cardiac rehabilitation) and Neurodevelopmental Therapy Rehabilitation services to restore function following illness, Hospital - Inpatient: After Deductible, Enrollee injury or surgery, limited to the following restorative pays 10% Plan Coinsurance therapies: occupational therapy, physical therapy, and speech therapy. Services are limited to those necessary to restore or Outpatient Services: After Deductible, Enrollee improve functional abilities when physical, sensori-perceptual pays 10% Plan Coinsurance and/or communication impairment exists due to injury, illness or surgery. Outpatient services require a prescription or order from a physician that reflects a written plan of care to restore function and must be provided by a rehabilitation team that may include a physician, nurse, physical therapist, occupational therapist, or speech therapist. Preauthorization is not required. Habilitative care includes Medically Necessary services or devices designed to help an Enrollee keep, learn, or improve skills and functioning for daily living. Services may include occupational therapy, physical therapy, speech therapy when prescribed by a physician. Examples include therapy for a child who is not walking or talking at the expected age. These services may include physical and occupational therapy, speech-language pathology and other services for people with disabilities in a variety of inpatient and/or outpatient settings. Limited to a combined total of 60 inpatient days and 60 outpatient visits per calendar year for all Rehabilitation, Habilitative care, and cardiac and pulmonary rehabilitation services. Neurodevelopmental therapy to restore or improve function including maintenance in cases where significant deterioration in the Enrollee’s condition would result without the services, limited to the following therapies: occupational therapy, physical therapy and speech therapy. There is no visit limit for Neurodevelopmental therapy. Services with mental health diagnoses are covered with no limit. Non-Emergency inpatient hospital services require Preauthorization. Cardiac rehabilitation is covered when clinical criteria are Outpatient Services: After Deductible, Enrollee met. pays 10% Plan Coinsurance Preauthorization is required after initial limit. Limited to a combined total of 60 inpatient days and 60 outpatient visits per calendar year for all Rehabilitation, Habilitative care, cardiac and pulmonary rehabilitation PEBB HMOHSA 2024 38
 Kaiser Permanente WA CDHP EOC (2024) Page 37 Page 39
Kaiser Permanente WA CDHP EOC (2024) Page 37 Page 39