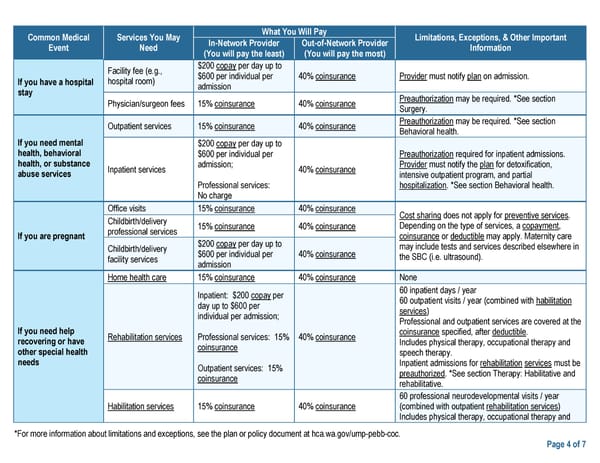
Common Medical Services You May What You Will Pay Limitations, Exceptions, & Other Important Event Need In-Network Provider Out-of-Network Provider Information (You will pay the least) (You will pay the most) Facility fee (e.g., $200 copay per day up to If you have a hospital hospital room) $600 per individual per 40% coinsurance Provider must notify plan on admission. stay admission Physician/surgeon fees 15% coinsurance 40% coinsurance Preauthorization may be required. *See section Surgery. Outpatient services 15% coinsurance 40% coinsurance Preauthorization may be required. *See section Behavioral health. If you need mental $200 copay per day up to health, behavioral $600 per individual per Preauthorization required for inpatient admissions. health, or substance Inpatient services admission; 40% coinsurance Provider must notify the plan for detoxification, abuse services intensive outpatient program, and partial Professional services: hospitalization. *See section Behavioral health. No charge Office visits 15% coinsurance 40% coinsurance Cost sharing does not apply for preventive services. Childbirth/delivery 15% coinsurance 40% coinsurance Depending on the type of services, a copayment, If you are pregnant professional services coinsurance or deductible may apply. Maternity care Childbirth/delivery $200 copay per day up to may include tests and services described elsewhere in facility services $600 per individual per 40% coinsurance the SBC (i.e. ultrasound). admission Home health care 15% coinsurance 40% coinsurance None Inpatient: $200 copay per 60 inpatient days / year day up to $600 per 60 outpatient visits / year (combined with habilitation individual per admission; services) If you need help Professional and outpatient services are covered at the recovering or have Rehabilitation services Professional services: 15% 40% coinsurance coinsurance specified, after deductible. other special health coinsurance Includes physical therapy, occupational therapy and needs speech therapy. Outpatient services: 15% Inpatient admissions for rehabilitation services must be coinsurance preauthorized. *See section Therapy: Habilitative and rehabilitative. 60 professional neurodevelopmental visits / year Habilitation services 15% coinsurance 40% coinsurance (combined with outpatient rehabilitation services) Includes physical therapy, occupational therapy and *For more information about limitations and exceptions, see the plan or policy document at hca.wa.gov/ump-pebb-coc. Page 4 of 7
 UMP Classic Medicare SBC (2024) Page 3 Page 5
UMP Classic Medicare SBC (2024) Page 3 Page 5