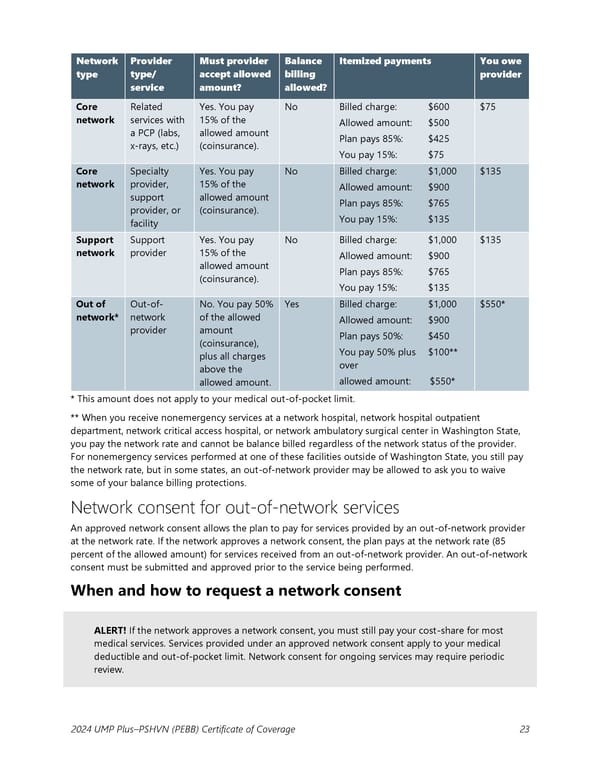
Network Provider Must provider Balance Itemized payments You owe type type/ accept allowed billing provider service amount? allowed? Core Related Yes. You pay No Billed charge: $600 $75 network services with 15% of the Allowed amount: $500 a PCP (labs, allowed amount Plan pays 85%: $425 x-rays, etc.) (coinsurance). You pay 15%: $75 Core Specialty Yes. You pay No Billed charge: $1,000 $135 network provider, 15% of the Allowed amount: $900 support allowed amount Plan pays 85%: $765 provider, or (coinsurance). You pay 15%: $135 facility Support Support Yes. You pay No Billed charge: $1,000 $135 network provider 15% of the Allowed amount: $900 allowed amount Plan pays 85%: $765 (coinsurance). You pay 15%: $135 Out of Out-of- No. You pay 50% Yes Billed charge: $1,000 $550* network* network of the allowed Allowed amount: $900 provider amount Plan pays 50%: $450 (coinsurance), You pay 50% plus $100** plus all charges over above the allowed amount: $550* allowed amount. * This amount does not apply to your medical out-of-pocket limit. ** When you receive nonemergency services at a network hospital, network hospital outpatient department, network critical access hospital, or network ambulatory surgical center in Washington State, you pay the network rate and cannot be balance billed regardless of the network status of the provider. For nonemergency services performed at one of these facilities outside of Washington State, you still pay the network rate, but in some states, an out-of-network provider may be allowed to ask you to waive some of your balance billing protections. Network consent for out-of-network services An approved network consent allows the plan to pay for services provided by an out-of-network provider at the network rate. If the network approves a network consent, the plan pays at the network rate (85 percent of the allowed amount) for services received from an out-of-network provider. An out-of-network consent must be submitted and approved prior to the service being performed. When and how to request a network consent ALERT! If the network approves a network consent, you must still pay your cost-share for most medical services. Services provided under an approved network consent apply to your medical deductible and out-of-pocket limit. Network consent for ongoing services may require periodic review. 2024 UMP Plus–PSHVN (PEBB) Certificate of Coverage 23
 UMP Plus–Puget Sound High Value Network (PSHVN) COC (2024) Page 23 Page 25
UMP Plus–Puget Sound High Value Network (PSHVN) COC (2024) Page 23 Page 25