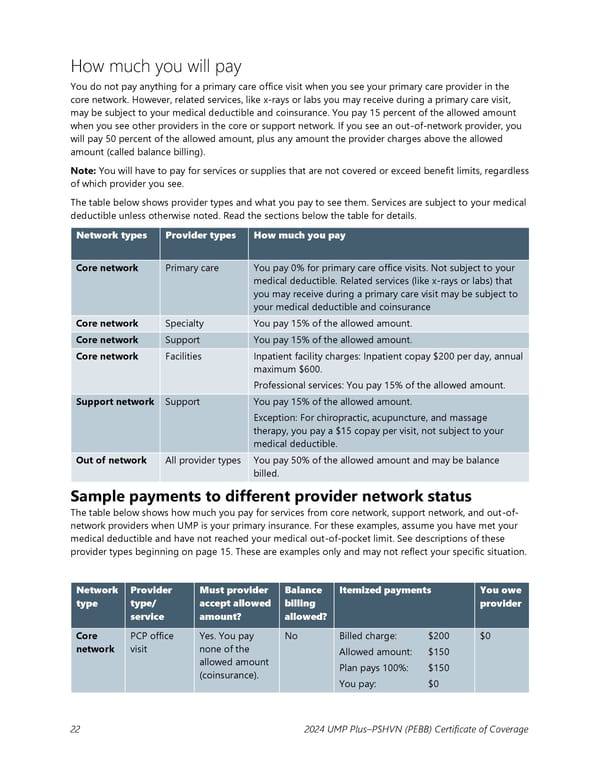
How much you will pay You do not pay anything for a primary care office visit when you see your primary care provider in the core network. However, related services, like x-rays or labs you may receive during a primary care visit, may be subject to your medical deductible and coinsurance. You pay 15 percent of the allowed amount when you see other providers in the core or support network. If you see an out-of-network provider, you will pay 50 percent of the allowed amount, plus any amount the provider charges above the allowed amount (called balance billing). Note: You will have to pay for services or supplies that are not covered or exceed benefit limits, regardless of which provider you see. The table below shows provider types and what you pay to see them. Services are subject to your medical deductible unless otherwise noted. Read the sections below the table for details. Network types Provider types How much you pay Core network Primary care You pay 0% for primary care office visits. Not subject to your medical deductible. Related services (like x-rays or labs) that you may receive during a primary care visit may be subject to your medical deductible and coinsurance Core network Specialty You pay 15% of the allowed amount. Core network Support You pay 15% of the allowed amount. Core network Facilities Inpatient facility charges: Inpatient copay $200 per day, annual maximum $600. Professional services: You pay 15% of the allowed amount. Support network Support You pay 15% of the allowed amount. Exception: For chiropractic, acupuncture, and massage therapy, you pay a $15 copay per visit, not subject to your medical deductible. Out of network All provider types You pay 50% of the allowed amount and may be balance billed. Sample payments to different provider network status The table below shows how much you pay for services from core network, support network, and out-of- network providers when UMP is your primary insurance. For these examples, assume you have met your medical deductible and have not reached your medical out-of-pocket limit. See descriptions of these provider types beginning on page 15. These are examples only and may not reflect your specific situation. Network Provider Must provider Balance Itemized payments You owe type type/ accept allowed billing provider service amount? allowed? Core PCP office Yes. You pay No Billed charge: $200 $0 network visit none of the Allowed amount: $150 allowed amount Plan pays 100%: $150 (coinsurance). You pay: $0 22 2024 UMP Plus–PSHVN (PEBB) Certificate of Coverage
 UMP Plus–Puget Sound High Value Network (PSHVN) COC (2024) Page 22 Page 24
UMP Plus–Puget Sound High Value Network (PSHVN) COC (2024) Page 22 Page 24