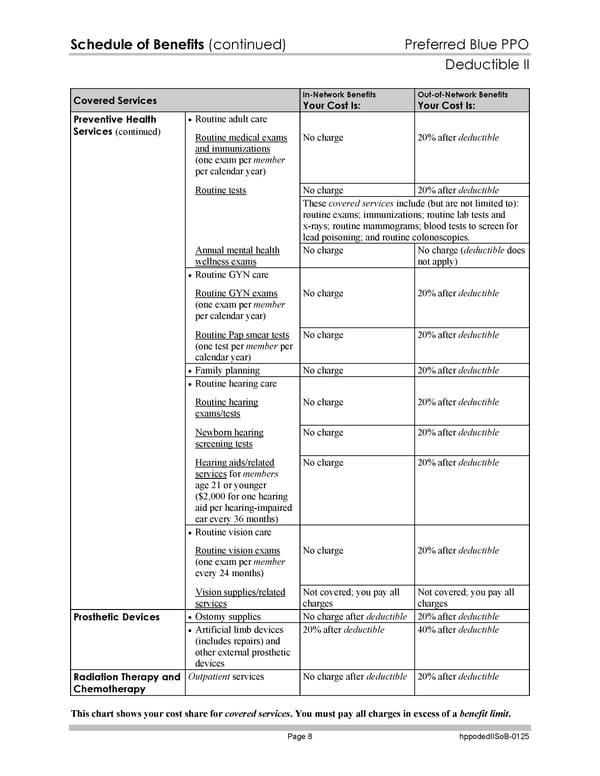
Schedule of Benefits (continued) Preferred Blue PPO Deductible II This chart shows your cost share for covered services. You must pay all charges in excess of a benefit limit. Page 8 hppodedIISoB-0125 Covered Services In-Network Benefits Your Cost Is: Out-of-Network Benefits Your Cost Is: Routine adult care Routine medical exams and immunizations (one exam per member per calendar year) No charge 20% after deductible No charge 20% after deductible Routine tests These covered services include (but are not limited to): routine exams; immunizations; routine lab tests and x-rays; routine mammograms; blood tests to screen for lead poisoning; and routine colonoscopies. Annual mental health wellness exams No charge No charge (deductible does not apply) Routine GYN care Routine GYN exams (one exam per member per calendar year) No charge 20% after deductible Routine Pap smear tests (one test per member per calendar year) No charge 20% after deductible Family planning No charge 20% after deductible Routine hearing care Routine hearing exams/tests No charge 20% after deductible Newborn hearing screening tests No charge 20% after deductible Hearing aids/related services for members age 21 or younger ($2,000 for one hearing aid per hearing-impaired ear every 36 months) No charge 20% after deductible Routine vision care Routine vision exams (one exam per member every 24 months) No charge 20% after deductible Preventive Health Services (continued) Vision supplies/related services Not covered; you pay all charges Not covered; you pay all charges Ostomy supplies No charge after deductible 20% after deductible Prosthetic Devices Artificial limb devices (includes repairs) and other external prosthetic devices 20% after deductible 40% after deductible Radiation Therapy and Chemotherapy Outpatient services No charge after deductible 20% after deductible
 Subscriber Certificate and Rider Documentation Page 134 Page 136
Subscriber Certificate and Rider Documentation Page 134 Page 136