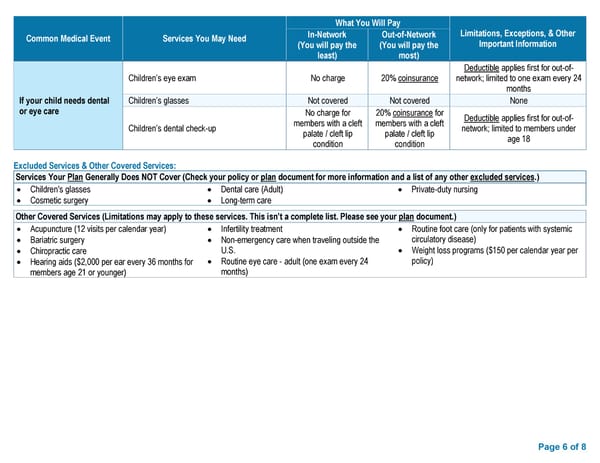
What You Will Pay Common Medical Event Services You May Need In-Network Out-of-Network Limitations, Exceptions, & Other (You will pay the (You will pay the Important Information least) most) Deductible applies first for out-of- Children’s eye exam No charge 20% coinsurance network; limited to one exam every 24 months If your child needs dental Children’s glasses Not covered Not covered None or eye care No charge for 20% coinsurance for Deductible applies first for out-of- Children’s dental check-up members with a cleft members with a cleft network; limited to members under palate / cleft lip palate / cleft lip age 18 condition condition Excluded Services & Other Covered Services: Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) • Children's glasses • Dental care (Adult) • Private-duty nursing • Cosmetic surgery • Long-term care Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) • Acupuncture (12 visits per calendar year) • Infertility treatment • Routine foot care (only for patients with systemic • Bariatric surgery • Non-emergency care when traveling outside the circulatory disease) • Chiropractic care U.S. • Weight loss programs ($150 per calendar year per • Hearing aids ($2,000 per ear every 36 months for • Routine eye care - adult (one exam every 24 policy) members age 21 or younger) months) Page 6 of 8
 Summary of Benefits and Coverage - Preferred Blue PPO $4000 Deductible II Page 5 Page 7
Summary of Benefits and Coverage - Preferred Blue PPO $4000 Deductible II Page 5 Page 7