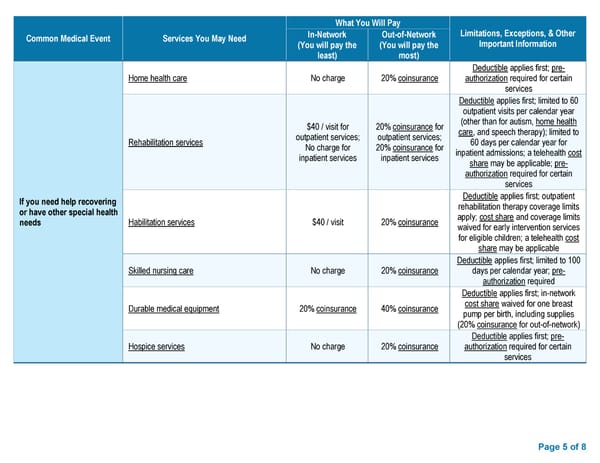
What You Will Pay Common Medical Event Services You May Need In-Network Out-of-Network Limitations, Exceptions, & Other (You will pay the (You will pay the Important Information least) most) Deductible applies first; pre- Home health care No charge 20% coinsurance authorization required for certain services Deductible applies first; limited to 60 outpatient visits per calendar year $40 / visit for 20% coinsurance for (other than for autism, home health outpatient services; outpatient services; care, and speech therapy); limited to Rehabilitation services No charge for 20% coinsurance for 60 days per calendar year for inpatient services inpatient services inpatient admissions; a telehealth cost share may be applicable; pre- authorization required for certain services If you need help recovering Deductible applies first; outpatient or have other special health rehabilitation therapy coverage limits needs Habilitation services $40 / visit 20% coinsurance apply; cost share and coverage limits waived for early intervention services for eligible children; a telehealth cost share may be applicable Deductible applies first; limited to 100 Skilled nursing care No charge 20% coinsurance days per calendar year; pre- authorization required Deductible applies first; in-network Durable medical equipment 20% coinsurance 40% coinsurance cost share waived for one breast pump per birth, including supplies (20% coinsurance for out-of-network) Deductible applies first; pre- Hospice services No charge 20% coinsurance authorization required for certain services Page 5 of 8
 Summary of Benefits and Coverage - Preferred Blue PPO $4000 Deductible II Page 4 Page 6
Summary of Benefits and Coverage - Preferred Blue PPO $4000 Deductible II Page 4 Page 6