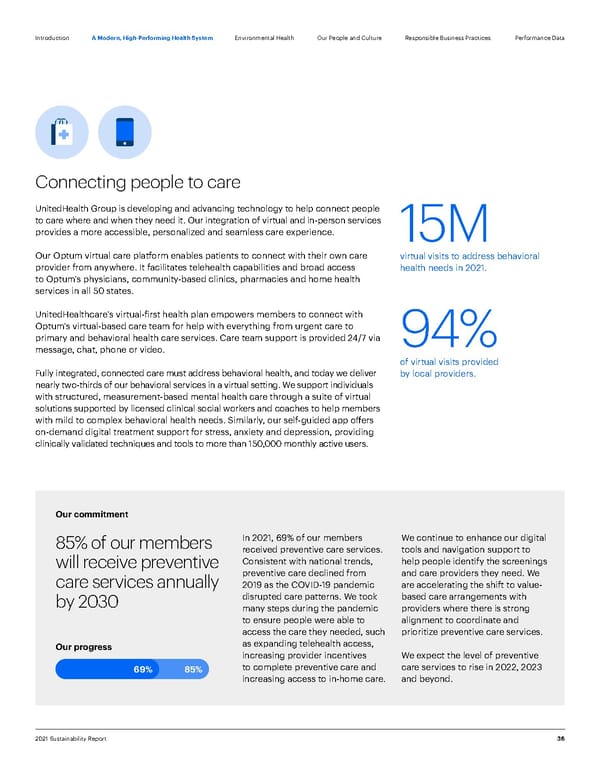
Introduction 36 2021 Sustainability Report A Modern, High-Performing Health System Our People and Culture Environmental Health Responsible Business Practices Performance Data 15M virtual visits to address behavioral health needs in 2021. 94% of virtual visits provided by local providers. Connecting people to care Our commitment 85% of our members will receive preventive care services annually by 2030 In 2021, 69% of our members received preventive care services. Consistent with national trends, preventive care declined from 2019 as the COVID-19 pandemic disrupted care patterns. We took many steps during the pandemic to ensure people were able to access the care they needed, such as expanding telehealth access, increasing provider incentives to complete preventive care and increasing access to in-home care. We continue to enhance our digital tools and navigation support to help people identify the screenings and care providers they need. We are accelerating the shift to value- based care arrangements with providers where there is strong alignment to coordinate and prioritize preventive care services. We expect the level of preventive care services to rise in 2022, 2023 and beyond. Our progress 69% 85% UnitedHealth Group is developing and advancing technology to help connect people to care where and when they need it. Our integration of virtual and in-person services provides a more accessible, personalized and seamless care experience. Our Optum virtual care platform enables patients to connect with their own care provider from anywhere. It facilitates telehealth capabilities and broad access to Optum’s physicians, community-based clinics, pharmacies and home health services in all 50 states. UnitedHealthcare’s virtual-first health plan empowers members to connect with Optum’s virtual-based care team for help with everything from urgent care to primary and behavioral health care services. Care team support is provided 24/7 via message, chat, phone or video. Fully integrated, connected care must address behavioral health, and today we deliver nearly two-thirds of our behavioral services in a virtual setting. We support individuals with structured, measurement-based mental health care through a suite of virtual solutions supported by licensed clinical social workers and coaches to help members with mild to complex behavioral health needs. Similarly, our self-guided app offers on-demand digital treatment support for stress, anxiety and depression, providing clinically validated techniques and tools to more than 150,000 monthly active users.
 ESG Report | UnitedHealth Group Page 35 Page 37
ESG Report | UnitedHealth Group Page 35 Page 37