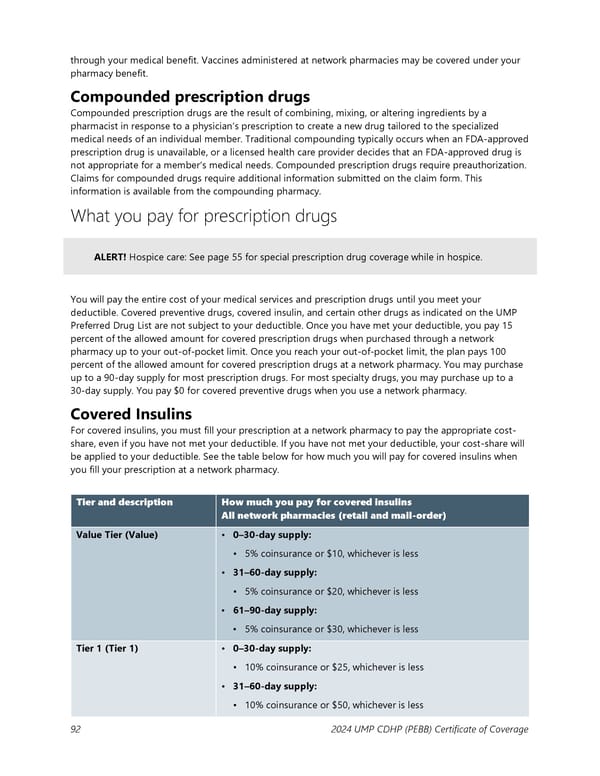
through your medical benefit. Vaccines administered at network pharmacies may be covered under your pharmacy benefit. Compounded prescription drugs Compounded prescription drugs are the result of combining, mixing, or altering ingredients by a pharmacist in response to a physician’s prescription to create a new drug tailored to the specialized medical needs of an individual member. Traditional compounding typically occurs when an FDA-approved prescription drug is unavailable, or a licensed health care provider decides that an FDA-approved drug is not appropriate for a member’s medical needs. Compounded prescription drugs require preauthorization. Claims for compounded drugs require additional information submitted on the claim form. This information is available from the compounding pharmacy. What you pay for prescription drugs ALERT! Hospice care: See page 55 for special prescription drug coverage while in hospice. You will pay the entire cost of your medical services and prescription drugs until you meet your deductible. Covered preventive drugs, covered insulin, and certain other drugs as indicated on the UMP Preferred Drug List are not subject to your deductible. Once you have met your deductible, you pay 15 percent of the allowed amount for covered prescription drugs when purchased through a network pharmacy up to your out-of-pocket limit. Once you reach your out-of-pocket limit, the plan pays 100 percent of the allowed amount for covered prescription drugs at a network pharmacy. You may purchase up to a 90-day supply for most prescription drugs. For most specialty drugs, you may purchase up to a 30-day supply. You pay $0 for covered preventive drugs when you use a network pharmacy. Covered Insulins For covered insulins, you must fill your prescription at a network pharmacy to pay the appropriate cost- share, even if you have not met your deductible. If you have not met your deductible, your cost-share will be applied to your deductible. See the table below for how much you will pay for covered insulins when you fill your prescription at a network pharmacy. Tier and description How much you pay for covered insulins All network pharmacies (retail and mail-order) Value Tier (Value) • 0–30-day supply: ▪ 5% coinsurance or $10, whichever is less • 31–60-day supply: ▪ 5% coinsurance or $20, whichever is less • 61–90-day supply: ▪ 5% coinsurance or $30, whichever is less Tier 1 (Tier 1) • 0–30-day supply: ▪ 10% coinsurance or $25, whichever is less • 31–60-day supply: ▪ 10% coinsurance or $50, whichever is less 92 2024 UMP CDHP (PEBB) Certificate of Coverage
 UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 92 Page 94
UMP Consumer-Directed Health Plan (CDHP) COC (2024) Page 92 Page 94