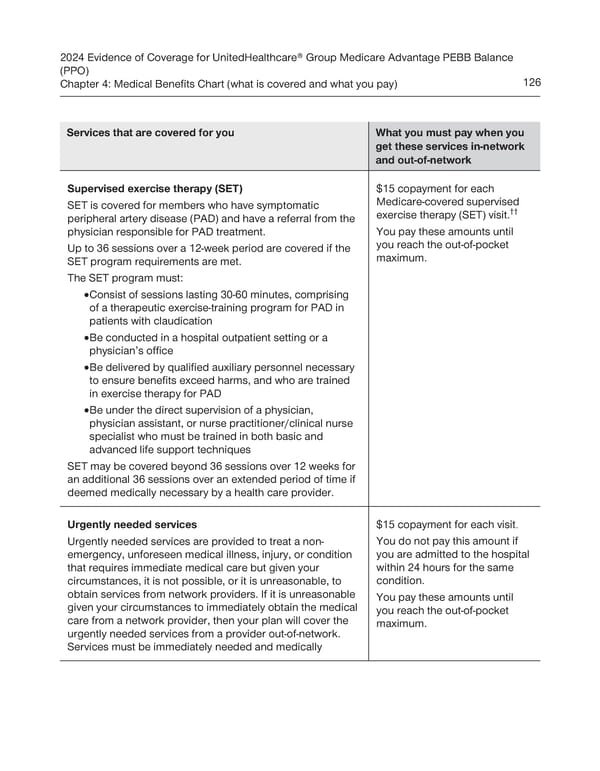
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Balance (PPO) Chapter 4: Medical Benefits Chart (what is covered and what you pay) 126 Services that are covered for you What you must pay when you get these services in-network and out-of-network Supervised exercise therapy (SET) $15 copayment for each SET is covered for members who have symptomatic Medicare-covered supervised exercise therapy (SET) visit.†† peripheral artery disease (PAD) and have a referral from the physician responsible for PAD treatment. You pay these amounts until Up to 36 sessions over a 12-week period are covered if the you reach the out-of-pocket SET program requirements are met. maximum. The SET program must: · Consist of sessions lasting 30-60 minutes, comprising of a therapeutic exercise-training program for PAD in patients with claudication · Be conducted in a hospital outpatient setting or a physician’s office · Be delivered by qualified auxiliary personnel necessary to ensure benefits exceed harms, and who are trained in exercise therapy for PAD · Be under the direct supervision of a physician, physician assistant, or nurse practitioner/clinical nurse specialist who must be trained in both basic and advanced life support techniques SET may be covered beyond 36 sessions over 12 weeks for an additional 36 sessions over an extended period of time if deemed medically necessary by a health care provider. Urgently needed services $15 copayment for each visit. Urgently needed services are provided to treat a non- You do not pay this amount if emergency, unforeseen medical illness, injury, or condition you are admitted to the hospital that requires immediate medical care but given your within 24 hours for the same circumstances, it is not possible, or it is unreasonable, to condition. obtain services from network providers. If it is unreasonable You pay these amounts until given your circumstances to immediately obtain the medical you reach the out-of-pocket care from a network provider, then your plan will cover the maximum. urgently needed services from a provider out-of-network. Services must be immediately needed and medically
 UnitedHealthcare PEBB Balance EOC (2024) Page 131 Page 133
UnitedHealthcare PEBB Balance EOC (2024) Page 131 Page 133