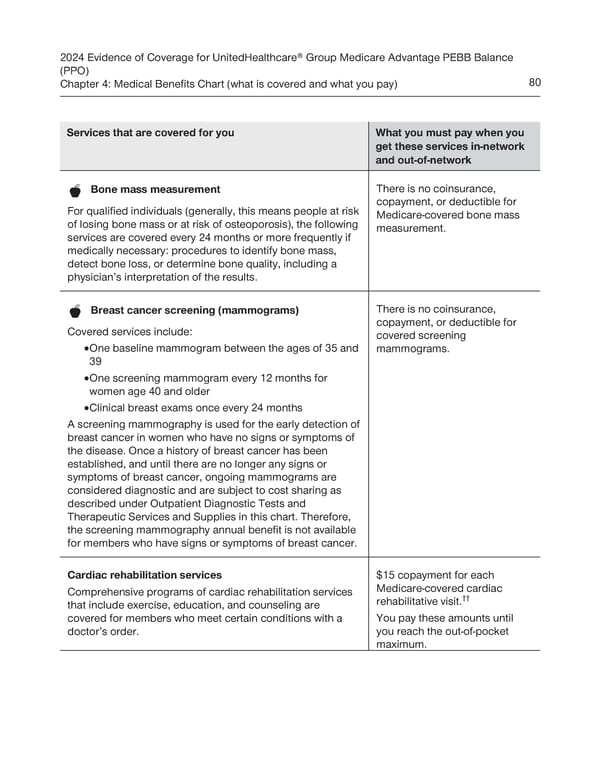
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Balance (PPO) Chapter 4: Medical Benefits Chart (what is covered and what you pay) 80 Services that are covered for you What you must pay when you get these services in-network and out-of-network There is no coinsurance, Bone mass measurement copayment, or deductible for For qualified individuals (generally, this means people at risk Medicare-covered bone mass of losing bone mass or at risk of osteoporosis), the following measurement. services are covered every 24 months or more frequently if medically necessary: procedures to identify bone mass, detect bone loss, or determine bone quality, including a physician’s interpretation of the results. There is no coinsurance, Breast cancer screening (mammograms) copayment, or deductible for Covered services include: covered screening · One baseline mammogram between the ages of 35 and mammograms. 39 · One screening mammogram every 12 months for women age 40 and older · Clinical breast exams once every 24 months A screening mammography is used for the early detection of breast cancer in women who have no signs or symptoms of the disease. Once a history of breast cancer has been established, and until there are no longer any signs or symptoms of breast cancer, ongoing mammograms are considered diagnostic and are subject to cost sharing as described under Outpatient Diagnostic Tests and Therapeutic Services and Supplies in this chart. Therefore, the screening mammography annual benefit is not available for members who have signs or symptoms of breast cancer. Cardiac rehabilitation services $15 copayment for each Comprehensive programs of cardiac rehabilitation services Medicare-covered cardiac rehabilitative visit.†† that include exercise, education, and counseling are covered for members who meet certain conditions with a You pay these amounts until doctor’s order. you reach the out-of-pocket maximum.
 UnitedHealthcare PEBB Balance EOC (2024) Page 85 Page 87
UnitedHealthcare PEBB Balance EOC (2024) Page 85 Page 87