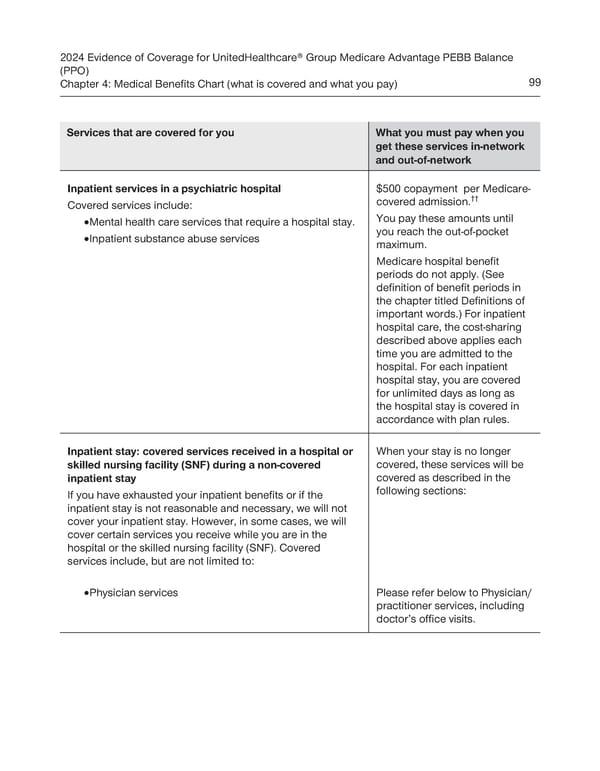
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Balance (PPO) Chapter 4: Medical Benefits Chart (what is covered and what you pay) 99 Services that are covered for you What you must pay when you get these services in-network and out-of-network Inpatient services in a psychiatric hospital $500 copayment per Medicare- covered admission.†† Covered services include: · Mental health care services that require a hospital stay. You pay these amounts until · Inpatient substance abuse services you reach the out-of-pocket maximum. Medicare hospital benefit periods do not apply. (See definition of benefit periods in the chapter titled Definitions of important words.) For inpatient hospital care, the cost-sharing described above applies each time you are admitted to the hospital. For each inpatient hospital stay, you are covered for unlimited days as long as the hospital stay is covered in accordance with plan rules. Inpatient stay: covered services received in a hospital or When your stay is no longer skilled nursing facility (SNF) during a non-covered covered, these services will be inpatient stay covered as described in the If you have exhausted your inpatient benefits or if the following sections: inpatient stay is not reasonable and necessary, we will not cover your inpatient stay. However, in some cases, we will cover certain services you receive while you are in the hospital or the skilled nursing facility (SNF). Covered services include, but are not limited to: · Physician services Please refer below to Physician/ practitioner services, including doctor’s office visits.
 UnitedHealthcare PEBB Balance EOC (2024) Page 104 Page 106
UnitedHealthcare PEBB Balance EOC (2024) Page 104 Page 106