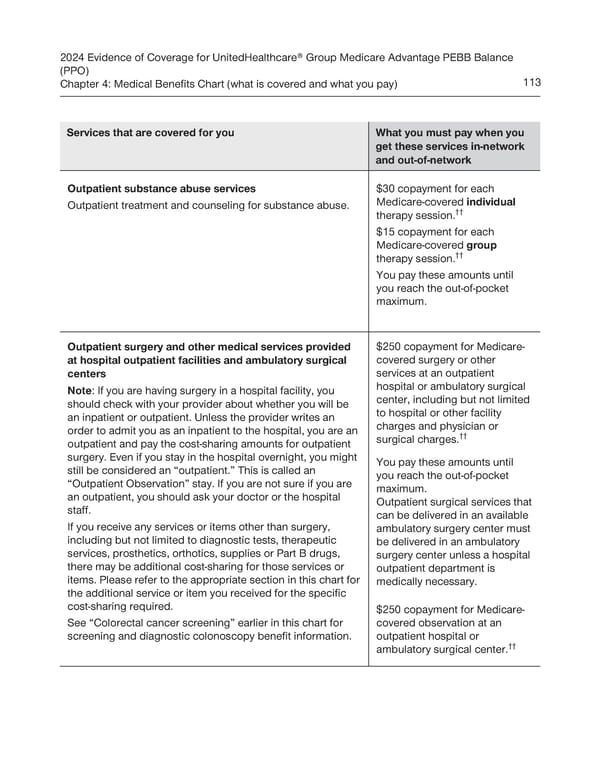
2024 Evidence of Coverage for UnitedHealthcare® Group Medicare Advantage PEBB Balance (PPO) Chapter 4: Medical Benefits Chart (what is covered and what you pay) 113 Services that are covered for you What you must pay when you get these services in-network and out-of-network Outpatient substance abuse services $30 copayment for each Outpatient treatment and counseling for substance abuse. Medicare-covered individual therapy session.†† $15 copayment for each Medicare-covered group therapy session.†† You pay these amounts until you reach the out-of-pocket maximum. Outpatient surgery and other medical services provided $250 copayment for Medicare- at hospital outpatient facilities and ambulatory surgical covered surgery or other centers services at an outpatient Note: If you are having surgery in a hospital facility, you hospital or ambulatory surgical should check with your provider about whether you will be center, including but not limited an inpatient or outpatient. Unless the provider writes an to hospital or other facility order to admit you as an inpatient to the hospital, you are an charges and physician or surgical charges.†† outpatient and pay the cost-sharing amounts for outpatient surgery. Even if you stay in the hospital overnight, you might You pay these amounts until still be considered an “outpatient.” This is called an you reach the out-of-pocket “Outpatient Observation” stay. If you are not sure if you are maximum. an outpatient, you should ask your doctor or the hospital Outpatient surgical services that staff. can be delivered in an available If you receive any services or items other than surgery, ambulatory surgery center must including but not limited to diagnostic tests, therapeutic be delivered in an ambulatory services, prosthetics, orthotics, supplies or Part B drugs, surgery center unless a hospital there may be additional cost-sharing for those services or outpatient department is items. Please refer to the appropriate section in this chart for medically necessary. the additional service or item you received for the specific cost-sharing required. $250 copayment for Medicare- See “Colorectal cancer screening” earlier in this chart for covered observation at an screening and diagnostic colonoscopy benefit information. outpatient hospital or ambulatory surgical center.††
 UnitedHealthcare PEBB Balance EOC (2024) Page 118 Page 120
UnitedHealthcare PEBB Balance EOC (2024) Page 118 Page 120